Wound Debridement — Types and Techniques for Faster, Safer Healing
Debridement is a core step in wound care: it removes dead, damaged, or infected tissue so healing can proceed. In this guide we walk through common debridement methods, when each is used, and how thoughtful technique improves outcomes. Whether you’re a clinician making treatment decisions or a patient learning your options, understanding debridement helps reduce infection risk and supports a healthy wound bed — the essential foundation for recovery. We also highlight how mobile wound care services bring expert debridement to patients who need care at home.
What is Wound Debridement and Why is It Essential?
Wound debridement is the clinical removal of necrotic (dead) tissue and foreign material from a wound to encourage healthy repair and limit infection. Clearing away this barrier creates a clean wound bed, improves local blood flow, and lets healthy tissue grow. Proper debridement can also lessen pain and speed recovery, especially in chronic or postoperative wounds. Knowing why and when to debride is a key part of effective wound management.
How Does Debridement Promote Wound Healing and Prevent Infection?
Debridement removes tissue and debris that block healing and harbor bacteria. With necrotic tissue gone, oxygen and nutrients reach the wound more easily, and the body can build granulation tissue. Removing bacteria-laden material lowers infection risk and, when done in a timely, appropriate manner, is associated with faster healing and better clinical outcomes.
What Role Does Debridement Play in Managing Chronic Wounds?
Chronic wounds — like diabetic foot ulcers or pressure injuries — often contain persistent necrotic tissue that stalls repair. Regular, targeted debridement helps keep the wound environment conducive to healing, encourages granulation, and can shift a non-healing wound back toward closure. Evidence shows consistent debridement improves healing rates for many patients with chronic wounds.
What Are the Main Types of Wound Debridement Methods?
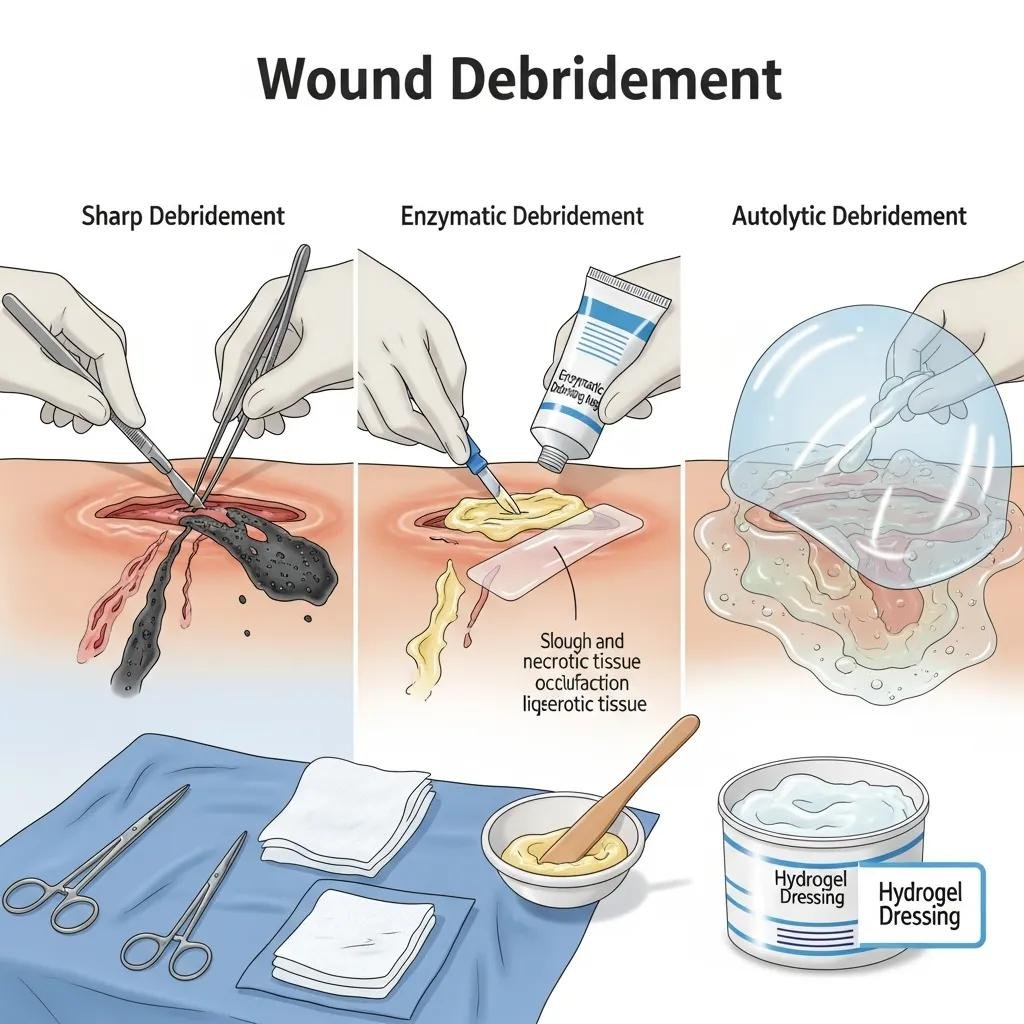
Clinicians choose a debridement method based on wound type, patient health, pain tolerance, and treatment goals. Below are the primary approaches, with a brief note on when each is typically used.
- Sharp Debridement
: Performed with scalpels or scissors to quickly remove necrotic tissue. Used when rapid, precise removal is needed and typically done by trained clinicians. - Enzymatic Debridement
: Topical enzyme preparations selectively break down dead tissue. Helpful for patients who cannot tolerate surgery or when a slower, selective approach is preferred. - Autolytic Debridement
: Uses the body’s own enzymes and moisture-retentive dressings to soften and remove dead tissue. A gentle option for stable wounds with low contamination. - Mechanical Debridement
: Physical removal of debris through methods such as irrigation or carefully applied wet-to-dry dressings and specialized tools. - Biological Debridement
: Sterile larvae (maggot therapy) selectively consume necrotic tissue and release enzymes that aid debridement and reduce bioburden. - Ultrasonic Debridement
: Low-frequency ultrasound is used to loosen and remove necrotic tissue with minimal trauma to healthy tissue.
| Debridement Type | Description | Indications |
|---|---|---|
| Sharp Debridement | Surgical removal of necrotic tissue with instruments | Large necrotic areas or urgent removal needs |
| Enzymatic Debridement | Topical enzyme agents that break down dead tissue | Patients who cannot undergo surgical debridement |
| Autolytic Debridement | Body’s own enzymes, supported by moisture-retentive dressings | Clean, stable wounds and sensitive skin |
| Mechanical Debridement | Physical cleansing via irrigation, dressings, or tools | Wounds with heavy debris or need for thorough cleaning |
| Biological Debridement | Sterile larvae that consume necrotic tissue selectively | Persistent, non-healing wounds where other methods failed |
| Ultrasonic Debridement | Low-frequency ultrasound to dislodge and remove necrotic tissue | Patients needing a less invasive, tissue-sparing option |
How Does Sharp or Surgical Debridement Work and When Is It Used?
Sharp debridement employs scalpels, scissors, or curettes to excise necrotic tissue quickly and precisely. It’s done by trained clinicians in a clinic or bedside setting and is preferred when large amounts of dead tissue must be removed or when infection needs prompt control. Sharp debridement is often used for wounds that don’t respond to conservative care or when immediate cleaning will improve outcomes.
What Are the Benefits and Applications of Enzymatic Debridement?
Enzymatic debridement uses topical products that selectively digest necrotic material while sparing viable tissue. It’s useful for patients who are poor surgical candidates or who require a more gradual, less invasive approach. These agents are straightforward to apply and can be managed in outpatient or home-care settings while maintaining a moist environment that supports healing.
Multiple studies support enzymatic agents as an effective option for chronic wound debridement when used appropriately.
Efficacy of Enzymatic Wound Debridement
Reviewers identified evidence that enzymatic debriding agents, alone or alongside serial conventional sharp wound debridement (CSWD), are effective for many patients with chronic wounds.
Enzymatic wound debridement, 2008
How Do Autolytic and Mechanical Debridement Techniques Differ?
Autolytic and mechanical debridement both remove necrotic tissue but rely on different mechanisms. Autolytic leverages the body’s own processes and dressings to soften and clear tissue slowly, while mechanical methods physically dislodge and remove material using irrigation, dressings, or devices.
What Is Autolytic Debridement and Which Wounds Benefit Most?
Autolytic debridement is best for wounds with limited contamination where a gentle, patient-friendly approach is appropriate. By keeping the wound moist with appropriate dressings, the body’s enzymes break down dead tissue over time. This approach minimizes pain and is well suited to patients with fragile skin or those who prefer a conservative strategy.
When Is Mechanical Debridement Appropriate and What Are Its Methods?
Mechanical debridement is chosen when a more active, thorough cleansing is needed. Techniques include irrigation under pressure, wet-to-dry dressings applied and removed to pull away debris, and use of specialized mechanical tools. It’s indicated for wounds with substantial necrotic burden or debris that impede healing.
What Are Biological and Ultrasonic Debridement Techniques?
Biological and ultrasonic techniques offer targeted alternatives to traditional methods. Each has distinct advantages depending on wound characteristics and patient preferences.
How Does Biological Debridement Using Maggot Therapy Work?
Biological debridement — commonly called maggot therapy — uses sterile larvae that digest necrotic tissue and secrete substances that help disinfect the wound. It can be especially effective for chronic wounds that have not responded to other approaches. Though the idea may be unfamiliar to some patients, controlled studies show maggot therapy can reduce necrotic tissue and support healing in select cases.
Growing evidence supports maggot debridement therapy as an option for certain chronic lower-extremity ulcers.
Maggot Debridement Therapy for Chronic Ulcers
This review examines maggot debridement therapy — its efficacy, application techniques, and safety for chronic lower-extremity ulcers. The evidence supports MDT as an effective treatment for some diabetic ulcers.
Reappraisal and updated review of maggot debridement therapy in chronic lower extremity ulcers, A Khachemoune, 2023
What Are the Advantages of Ultrasonic Debridement in Wound Care?
Ultrasonic debridement uses low-frequency sound waves to loosen and remove necrotic tissue while preserving healthy tissue. It’s less invasive than surgical excision and can reduce patient discomfort. Ultrasonic devices can also target specific areas, making them useful for wounds where precision and tissue preservation are priorities.
Emerging technologies — including hydrosurgery and ultrasound devices — offer promising, tissue-sparing alternatives for chronic wound debridement.
Advanced Debridement Techniques for Chronic Wounds
Debridement remains central to wound management. Newer modalities like hydrosurgery (Versajet), ultrasound therapy (MIST), and plasma-mediated ablation (Coblation) offer selective, efficient debridement. Hydrosurgery can speed tissue removal, ultrasound can reduce exudate, and these technologies may improve healing times for chronic wounds.
New techniques for wound management: A systematic review of their role in the management of chronic wounds, 2018
How Does Mobile Wound Debridement Enhance Patient Care?

Mobile debridement brings specialized wound care to the patient’s home, removing travel barriers and delivering treatment in a familiar setting. This model helps patients with limited mobility, transportation challenges, or those who prefer care at home.
What Are the Benefits of Receiving Debridement Services at Home?
Home-based debridement offers comfort, reduces stress from travel, and enables more personalized, frequent follow-up. Clinicians can tailor treatments to the patient’s living situation and support better adherence to care plans, which often improves outcomes.
How Does Healix360 Provide Expert Mobile Debridement Services?
Healix360 Advanced Mobile Wound Care Specialists
provide on‑site wound assessments and individualized debridement plans delivered by trained clinicians. We combine evidence-based techniques with practical, patient-centered care to support safer, faster healing — whether that care happens in clinic, at bedside, or in your home.
What Should Patients Expect During and After Debridement Procedures?
Before any debridement, clinicians assess the wound, review medical history, and discuss the chosen method and pain-control plan. Clear expectations and informed consent help reduce anxiety and improve the care experience.
How Is Pain Managed Across Different Debridement Techniques?
Pain control is tailored to the method and patient needs. Providers may use topical or local anesthetics, oral analgesics, or comfort measures to minimize discomfort. The goal is safe, effective debridement with the least pain possible.
What Are the Key Steps in Post-Debridement Wound Care and Monitoring?
After debridement, follow-up care focuses on infection prevention and promoting tissue repair. Key steps include appropriate dressing selection, wound hygiene, monitoring for signs of infection, and scheduled reassessments. Follow your clinician’s instructions and report any concerning changes promptly.
For questions about mobile wound care or to schedule a consultation, please contact
Healix360
.
Frequently Asked Questions
What are the signs that a wound may need debridement?
Signs that debridement may be needed include visible necrotic (dead) tissue, a persistent foul odor, increased or unusual drainage, and stalled healing. Redness, swelling, pus, or increasing pain can also indicate infection and the need for clinical evaluation.
How often should debridement be performed on chronic wounds?
Frequency depends on the wound and the method used. Sharp debridement is often scheduled weekly or biweekly when needed, while enzymatic or autolytic approaches are applied based on progress and clinician assessment. Your care team will set a schedule that balances healing benefit with patient comfort.
Can patients perform debridement at home?
Some conservative methods, like enzymatic or autolytic care, may be managed at home under professional guidance. However, more invasive techniques should only be performed by trained clinicians. Always consult your provider before attempting any self-debridement to avoid harm.
What are the risks associated with wound debridement?
Debridement carries potential risks, including pain, bleeding, and infection. Improper technique can damage healthy tissue or delay healing. Patients with diabetes, poor circulation, or immune compromise may face higher risks and require careful monitoring by experienced clinicians.
How can patients prepare for a debridement procedure?
Prepare by sharing your full medical history and medication list, following any pre-procedure instructions (for example about blood thinners), and discussing pain-management preferences. Asking questions ahead of time helps ensure you’re comfortable and informed.
What should patients do if they notice complications after debridement?
Contact your healthcare provider promptly if you see increasing redness, swelling, new or worsening drainage, fever, or unexpected pain. Early communication lets clinicians address infections or other complications quickly to protect healing.
Conclusion
Debridement is a foundational step in effective wound care: it clears barriers to healing, lowers infection risk, and helps the body rebuild healthy tissue. Understanding the available methods — and working with experienced clinicians — ensures the right approach for each wound and patient. Mobile wound care services like Healix360 make expert debridement and follow-up more accessible, so more patients receive timely, individualized care. To learn more about improving your wound care plan, explore our services or reach out for a consultation.







