Surgical Wound Care: A Practical Guide to Post‑Operative Healing and Management
Surgical wound care strongly shapes recovery — from how quickly tissue heals to how comfortable you feel after surgery. This guide walks through the essentials: common wound types, the healing stages, how to spot and prevent infection, advanced treatment options, and why mobile wound care can make a difference. These insights are designed for patients and caregivers who want clear, practical information to avoid complications and speed recovery. We also explain how Healix360 Advanced Mobile Wound Care Specialists deliver personalized, advanced care that supports better outcomes.
What Are Surgical Wounds and How Do They Affect Recovery?
Surgical wounds are the incisions made during an operation. How these wounds are cared for after surgery affects infection risk, scarring, pain, and overall recovery time. Knowing the different wound types and their unique care needs helps you and your care team take the right steps during the post‑operative period.
What Types of Surgical Incisions Require Special Care?
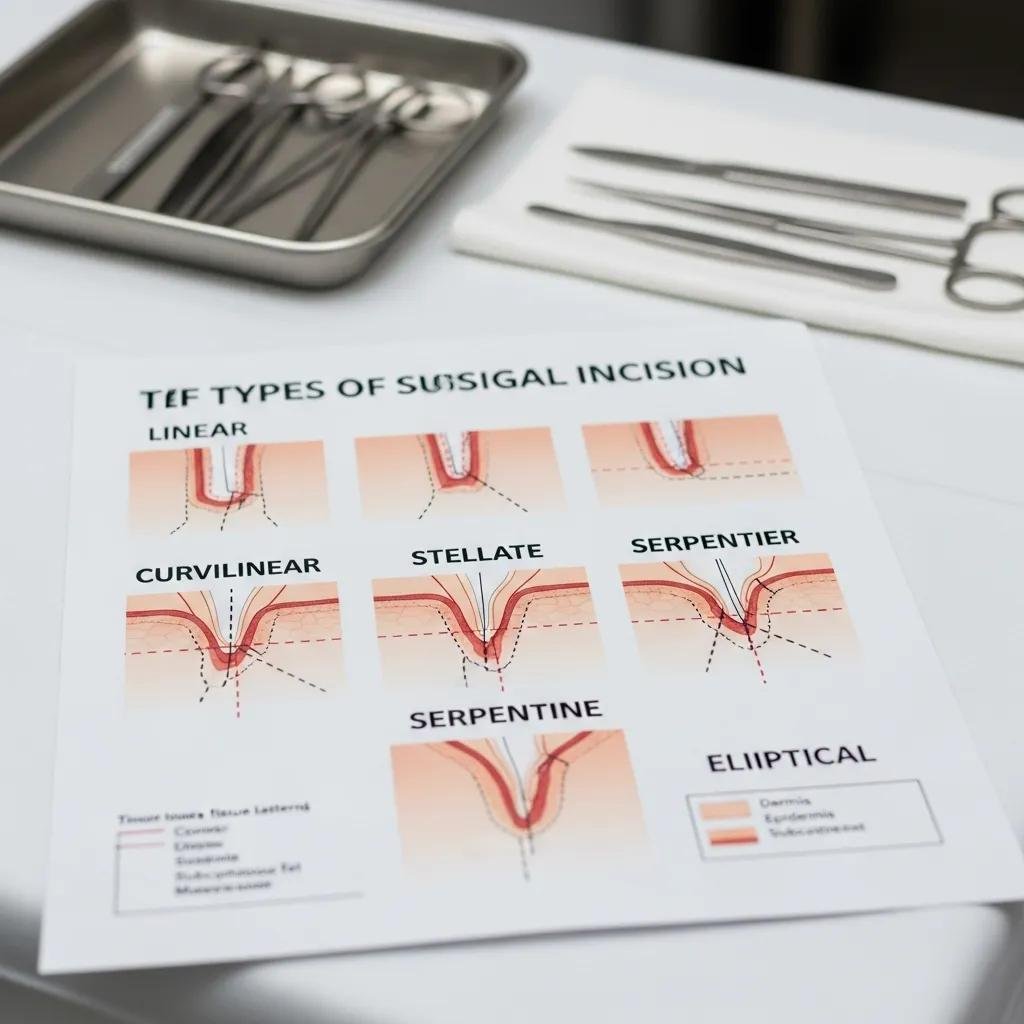
Some incisions need closer attention because of where they’re located, how deep they are, or the patient’s health. For example, deep abdominal cuts usually require more careful monitoring than a small skin incision. Incisions near joints or areas of frequent motion are also at higher risk for reopening or delayed healing. Good post‑op care includes regular checks, following hygiene instructions, and working with your care team to reduce risks.
Which Risk Factors Influence Surgical Wound Healing?
Several factors can slow healing or raise complication risk:
- Diabetes: High blood sugar can reduce circulation and slow tissue repair.
- Obesity: Extra tension on the wound and reduced blood flow can impede healing.
- Smoking: Nicotine narrows blood vessels and lowers oxygen delivery to tissue.
When possible, addressing these risks — with medical guidance and lifestyle changes — improves recovery and reduces complications.
What Are the Stages of Surgical Wound Healing and Typical Timelines?
What Happens During Each Phase of Wound Healing After Surgery?
Wound healing progresses through four main phases:
- Hemostasis: Right after surgery your body forms clots to stop bleeding.
- Inflammation: White blood cells clean the wound and protect against infection.
- Proliferation: New tissue and blood vessels grow to fill the wound.
- Remodeling: Over weeks to months the tissue strengthens and refines.
Each phase plays a necessary role; interruptions or infection at any stage can delay recovery.
How Long Does It Take for Surgical Incisions to Heal?
Surface healing of most surgical incisions is often apparent within 10 to 14 days, but deeper healing and full tissue strength can take weeks to months depending on the procedure and individual health. Age, overall medical condition, and how closely post‑op care instructions are followed all influence timelines.
How Can You Prevent and Recognize Surgical Wound Infections?
What Are the Common Symptoms of Surgical Wound Infection?
Watch for these common signs of infection around a surgical site:
- Redness: Increasing redness spreading from the incision.
- Swelling: Noticeable puffiness or hardening around the wound.
- Pus: Thick, discolored drainage or an unpleasant odor.
Early recognition and prompt treatment make infections easier to manage and reduce the chance of serious complications.
Which Strategies Help Prevent Post-Operative Wound Complications?
Practical steps to lower complication risk include:
- Maintain hygiene: Clean the wound exactly as your care team recommends.
- Follow care instructions: Keep appointments and follow dressing, activity, and medication guidance.
- Monitor for symptoms: Check the site daily and call your provider if you see signs of infection.
These simple, consistent actions support safer healing and better outcomes.
Clinical guidance consistently emphasizes strict infection‑prevention practices in post‑operative care.
Post-Operative Infection Prevention & Surgical Site Care
Background: To address gaps in infection‑prevention practices, national agencies partnered to standardize measures and improve consistency in surgical site care.
What Advanced Treatments Are Available for Surgical Wound Care?
How Does Debridement Promote Healing in Surgical Wounds?
Debridement removes dead, damaged, or infected tissue so healthy tissue can grow. It lowers infection risk and creates a cleaner wound bed for healing. Depending on the wound’s condition, debridement may be surgical or performed using less invasive techniques under clinical supervision.
What Are the Benefits of Negative Pressure Wound Therapy and Biologic Dressings?

Advanced options like negative pressure wound therapy (NPWT) and biologic dressings offer specific advantages:
- Negative Pressure Wound Therapy: Uses controlled suction to remove fluid, increase blood flow, and encourage healthy granulation tissue.
- Biologic Dressings: Maintain a moist healing environment and may supply growth factors that support tissue regeneration.
These approaches are especially helpful for complex or slow‑healing wounds and are selected by clinicians based on each patient’s needs.
Research continues into engineered dressings and their role in improving surgical wound reconstruction.
Biologic Dressings for Surgical Wound Reconstruction
A review of biologic dressings explores their use for acute surgical wounds and reconstructive procedures, noting potential benefits and current limitations.
What Are the Benefits of Mobile Wound Care for Post-Surgery Recovery?
How Does Mobile Wound Care Improve Patient Comfort and Outcomes?
Mobile wound care brings professional treatment to your home, removing travel stress and long clinic waits. This convenience helps patients stick to care plans, reduces disruption during recovery, and often improves satisfaction and adherence — all of which support better healing.
Evidence supports mobile wound care models, including telemedicine, as effective ways to extend specialized care beyond clinic walls.
Mobile Wound Healing Centers & Telemedicine
Clinical teams with specialized training have implemented mobile wound‑healing models that combine in‑person visits and remote follow‑up to reach more patients efficiently.
How Does Mobile Care Support Caregivers and Reduce Hospital Visits?
Mobile wound care eases the burden on family caregivers by providing skilled clinicians at home for dressing changes, assessments, and education. That support reduces unnecessary clinic or ER visits and helps keep recovery on track with timely interventions.
How Does Healix360 Personalize Surgical Wound Care for Optimal Healing?
What Role Do Board-Certified Specialists Play in Customized Treatment Plans?
Our board‑certified specialists evaluate each patient’s history and wound characteristics to create tailored treatment plans. That expertise ensures the interventions — from dressing selection to advanced therapies — match the patient’s goals and clinical needs.
How Does Medicare Part B Coverage Facilitate Access to Advanced Wound Care?
Medicare Part B can cover many advanced wound care services, including certain in‑home treatments. This coverage helps make necessary therapies more accessible and reduces financial barriers to timely, effective care.
| Treatment Type | Overview | Benefits |
|---|---|---|
| Debridement | Removal of dead, damaged, or infected tissue to create a healthier wound bed | Encourages healthy tissue growth and lowers infection risk |
| Negative Pressure Therapy | Controlled suction applied to the wound to manage fluids and stimulate granulation | Improves blood flow and accelerates healing in complex wounds |
| Biologic Dressings | Advanced dressings that support a moist healing environment and may provide growth factors | Supports tissue regeneration and can improve repair quality |
Caring well for surgical wounds affects the whole recovery process. Knowing wound types, the healing timeline, and available treatments helps patients and caregivers take proactive steps. Mobile wound care from teams like Healix360 adds convenience and specialist attention, which can improve adherence and outcomes across the recovery journey.
Frequently Asked Questions
What should I do if I notice signs of infection in my surgical wound?
If you see growing redness, increased swelling, foul or colored drainage, or a fever, contact your healthcare provider right away. Early assessment lets clinicians catch infections sooner and start treatments — such as antibiotics or wound care adjustments — before complications develop. Don’t try to manage a suspected infection on your own; seek professional guidance.
How can I manage pain associated with surgical wounds during recovery?
Follow your provider’s pain‑management plan. Over‑the‑counter options like acetaminophen or ibuprofen can help for mild to moderate pain; your clinician may prescribe stronger medication if needed. Cold packs and elevation (when appropriate) can reduce swelling and discomfort. Always check with your care team before combining medications or using local therapies.
What lifestyle changes can support better surgical wound healing?
Support healing with a balanced diet rich in protein and vitamin C, adequate hydration, and, when cleared by your surgeon, gentle activity to promote circulation. Quit or avoid smoking, as it impairs blood flow. Work with your clinicians to manage chronic conditions like diabetes that affect healing.
How often should I change the dressing on my surgical wound?
Follow the specific instructions given by your surgeon or wound clinician. Dressings generally should be changed if they become wet, soiled, or loose. Some advanced dressings remain in place longer under clinical supervision. Always wash your hands before and after dressing changes, and contact your care team if you’re unsure.
What are the potential complications of improper wound care?
Poor wound care can lead to infection, delayed healing, increased scarring, or chronic wounds that need more intensive treatment. Systemic infections are a serious risk if local infections go untreated. To avoid these issues, follow post‑op instructions closely and reach out to your provider with any concerns.
Can I shower or bathe with a surgical wound?
Whether you can shower or bathe depends on the surgery and your provider’s instructions. Many wounds should be kept dry for the first few days; afterward, gentle washing with mild soap and water may be allowed, avoiding direct, forceful water on the incision. Always follow your surgeon’s guidance to protect healing.
Conclusion
Thoughtful surgical wound care matters. Understanding wound types, the healing process, infection signs, and advanced treatment options empowers patients and caregivers to act early and wisely. Mobile, specialist-led care from Healix360 brings targeted, convenient support that helps keep recovery on track. When you’re ready, explore our advanced wound care services to find the right plan for your recovery.







