Biofilm in Chronic Wounds: Detection and Advanced Mobile Treatment Options
Biofilm in chronic wounds is a common, stubborn barrier to healing that can cause prolonged pain and setbacks for patients. This guide breaks down what biofilm is, how clinicians spot it, and which evidence-based treatments work best — including modern mobile care options that bring treatment to the patient. Chronic wounds like diabetic foot ulcers and pressure injuries are especially prone to biofilm, which complicates recovery. Whether you’re a patient or a healthcare provider, this article explains the mechanisms, the diagnostics, and practical treatment strategies that improve outcomes.
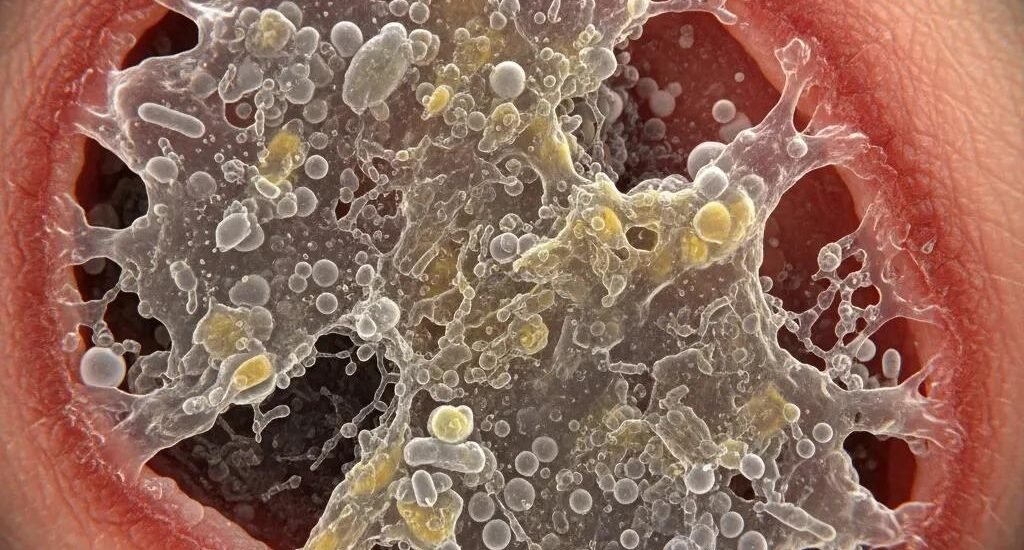
What is Biofilm and How Does it Impact Chronic Wound Healing?
Biofilm is a community of microbes — bacteria and sometimes fungi — embedded in a self-made protective matrix that adheres to tissue and wound surfaces. That matrix shields microbes from the immune system and many treatments, so infections can linger and healing stalls. In chronic wounds, biofilm contributes to ongoing inflammation, repeated infections, and tissue breakdown, all of which slow or stop repair.
How Does Biofilm Form in Chronic Wounds?
Biofilm usually starts when microbes attach to the wound bed, encouraged by moisture, nutrients, and factors such as poor circulation or diabetes. Once attached, microbes produce extracellular polymers that glue cells together and form a protective layer. Mixed communities — bacteria alongside fungi — cooperate inside this matrix, making it much harder for standard topical agents or antibiotics to clear the infection.
Why Does Biofilm Delay Wound Healing?
Biofilm delays healing in several ways. Its dense matrix limits immune cells and antibiotics from reaching microbes, allowing infection to persist. Some biofilm communities release enzymes and toxins that damage surrounding tissue. And the ongoing immune response produces chronic inflammation, which interferes with normal repair processes. Targeted approaches are needed to break that cycle and let healing resume.
How Do Specialists Detect Biofilm in Chronic Wounds?
Accurate detection guides treatment. Clinicians use a mix of bedside assessment and advanced tools to determine whether biofilm is present and how extensive it is.
What Clinical Signs Indicate Biofilm Presence?
Common clinical clues include wounds that drain persistently, heal very slowly despite care, or emit a noticeable odor. Increased local redness, swelling, and tissue breakdown despite appropriate therapy are additional red flags. Recognizing these signs early helps clinicians pursue diagnostic testing and escalate treatment when needed.
Which Advanced Diagnostic Techniques Are Used for Biofilm Detection?

Advanced methods include imaging and molecular tests. Imaging such as ultrasound or confocal laser scanning microscopy can visualize biofilm structure and burden; MRI may be used to evaluate deeper soft-tissue involvement in complex cases. Molecular tools like PCR identify specific pathogens within the biofilm. Together, these techniques enable more precise, individualized treatment plans.
Detecting and Treating Biofilm in Chronic Wounds with Mobile Care
Managing biofilm requires a layered strategy that both removes the biofilm and supports the wound’s recovery.
- Debridement: Physically removing necrotic tissue and the biofilm layer helps reset the wound environment and allows topical and systemic treatments to reach remaining microbes. Clinicians choose sharp, enzymatic, autolytic, or mechanical methods based on the wound and the patient.
- Biologic Dressings: These products maintain a moist healing environment, deliver growth factors, and provide a scaffold for tissue regrowth. When used appropriately, biologic dressings support healing and help protect the wound from new contamination.
- Antimicrobial Therapies: Topical antimicrobials, antiseptics, and when indicated systemic antibiotics reduce microbial load. Selecting agents and delivery methods that penetrate the biofilm matrix improves chances of eradication.
Evidence supports combining conventional care with targeted, anti-biofilm tactics — a layered approach increases the likelihood of durable healing.
Anti-Biofilm Strategies for Chronic Wound Care
ABSTRACT: With aging and rising rates of obesity, chronic wounds — including diabetic, pressure, and venous leg ulcers — are growing clinical challenges. Recognition of bacterial biofilm as a key factor in non-healing wounds has prompted calls for biofilm‑targeted care. Core elements of current care that remain important include systemic and topical antimicrobials, antiseptics, and physical debridement of devitalized tissue. Emerging strategies focus on improved, less invasive physical removal of biofilm, new chemical agents, and biological approaches that target biofilm specifically. Continued innovation is necessary to address the evolving wound-care burden.
How Does Debridement Disrupt Biofilm?
Debridement physically removes the protective matrix and the microbes it contains, exposing the wound bed to topical agents and the immune response. Regular, appropriate debridement is a cornerstone of biofilm management because it helps restart the healing trajectory and improves penetration of therapies.
What Role Do Biologic Dressings and Skin Substitutes Play?
Biologic dressings and skin substitutes supply a framework for new tissue growth and provide growth factors and nutrients that support repair. They help preserve a controlled, moist environment and can reduce the risk of reinfection when used alongside debridement and antimicrobial measures.
How Do Advanced Therapies Enhance Biofilm Wound Healing?
Advanced therapies add tools that target both the wound environment and the biofilm itself, improving outcomes where standard care alone is insufficient.
How Does Negative Pressure Wound Therapy Support Biofilm Management?
Negative pressure wound therapy (NPWT) applies controlled suction to remove fluid, reduce edema, and stimulate blood flow and granulation. By evacuating exudate and contaminants, NPWT can lower bacterial burden and disrupt biofilm architecture, helping the wound move toward closure.
Clinical research supports NPWT’s role in reducing biofilm burden and improving healing when applied early and correctly.
NPWT for Biofilm Prevention in Contaminated Wounds
ABSTRACT: Studies evaluating early NPWT application after wound contamination show reductions in biofilm matrix and bacterial counts compared with untreated controls. In animal models, continuous negative pressure initiated soon after contamination limited biofilm maturation and improved healing metrics. These findings suggest a preventive as well as therapeutic role for NPWT in certain contaminated wounds.
What Regenerative Medicine Options Are Available for Biofilm-Affected Wounds?
Regenerative approaches such as stem cell therapies and platelet‑rich plasma (PRP) aim to boost the body’s repair mechanisms by delivering concentrated cells and growth factors. Early data indicate potential benefits for healing chronic wounds, but high-quality trials are still needed to define their role specifically for biofilm‑related wounds.
Why Choose Mobile Wound Care for Biofilm Treatment?

Mobile wound care brings skilled clinicians, diagnostics, and evidence-based treatments to the patient’s home — improving access, comfort, and continuity of care for those managing chronic wounds and biofilm.
How Does In-Home Care Improve Biofilm Management?
In-home care enables frequent, tailored interventions: timely debridement, dressing changes, therapy adjustments, and close monitoring for signs of reinfection. That personalized attention helps catch problems early and keeps treatment aligned with the wound’s progress. Learn more about how we tailor plans on our contact page.
What Can Patients and Caregivers Expect During Mobile Biofilm Treatment?
Mobile care visits typically include a full wound assessment, appropriate debridement, selection of dressings or advanced therapies, patient and caregiver education, and a clear follow-up plan. Providers focus on practical instruction so home caregivers can support recovery between visits.
How Can Patients Prevent Biofilm Recurrence and Promote Healing at Home?
Preventing recurrence depends on consistent wound care, good overall health management, and early recognition of trouble signs.
- Maintain Proper Wound Hygiene: Follow clinician-directed cleaning and dressing schedules to reduce contamination risk.
- Monitor for Signs of Infection: Report increased redness, swelling, new or heavier drainage, or a change in odor promptly.
- Follow Nutritional Guidelines: Adequate protein, vitamins (especially C and zinc), and hydration support tissue repair and immune function.
What Practical Tips Help Prevent Biofilm Reformation?
Practical daily habits make a difference:
- Daily Care Routines: Keep a consistent schedule for cleaning, dressing changes, and skin checks.
- Signs to Monitor: Track changes in pain, drainage, color, or odor and document progress between visits.
- When to Seek Help: Contact your care team if you notice worsening signs or if the wound stops improving despite treatment.
What Are Common FAQs About Biofilm and Chronic Wound Care?
Patients frequently ask about causes, signs, and treatments for biofilm. Below are concise answers to common concerns.
- What is biofilm?: A protective community of microbes on the wound surface that resists treatments and slows healing.
- How can I tell if my wound has biofilm?: Look for persistent drainage, stalled healing, or an unusual odor despite proper care.
- What treatments are available for biofilm?: Combining debridement, appropriate antimicrobials, biologic dressings, and advanced therapies like NPWT offers the best chance for success.
| Treatment Option | Mechanism | Effectiveness |
|---|---|---|
| Debridement | Physically removes necrotic tissue and biofilm | High |
| Biologic Dressings | Maintain moist environment and deliver growth factors | Moderate |
| Negative Pressure Therapy | Removes exudate and improves perfusion | High |
This snapshot highlights how combining mechanical removal, supportive dressings, and therapies that improve wound physiology delivers the strongest results against biofilm.
Frequently Asked Questions
What are the long-term effects of biofilm on chronic wounds?
Left unchecked, biofilm can cause ongoing infection, chronic inflammation, delayed healing, and increased risk of tissue loss. These complications may require more intensive interventions and extend recovery time. Early, consistent treatment reduces long-term harm and improves quality of life.
How can patients recognize the signs of biofilm recurrence?
Watch for renewed or increased drainage, a bad odor, more redness or swelling, and a wound that stops progressing or worsens despite treatment. Any unexpected change should prompt contact with your care team for reassessment.
What lifestyle changes can support wound healing and prevent biofilm?
Good nutrition, staying hydrated, controlling blood sugar, avoiding tobacco, and following wound-care instructions all support healing. Managing underlying conditions like diabetes and maintaining mobility and circulation also reduce biofilm risk.
Are there any emerging treatments for biofilm in chronic wounds?
Research is active in areas such as photodynamic therapy, bacteriophage therapy, and regenerative medicine tools like stem cells and PRP. These show promise, but many need more clinical evidence before routine use for biofilm-specific care.
How does patient education play a role in managing biofilm?
Education empowers patients and caregivers to follow treatment plans correctly, recognize early signs of trouble, and maintain preventive routines. Clear, practical instruction improves adherence and outcomes.
What is the role of telehealth in managing chronic wounds affected by biofilm?
Telehealth provides timely access to clinicians for visual checks, guidance between visits, and early troubleshooting. While it doesn’t replace in-person procedures like debridement, telehealth enhances follow-up, supports adherence, and speeds intervention when needed.
Conclusion
Biofilm complicates many chronic wounds, but a deliberate, multi-pronged approach — accurate detection, regular debridement, targeted antimicrobials, supportive dressings, and advanced therapies when appropriate — improves the chances of healing. Mobile wound care delivers these elements where patients are, helping sustain treatment and catch setbacks early. Stay engaged with your care team, follow recommended routines, and reach out promptly if your wound stops improving.