Your Mobile Wound Care Guide — Understand your plan and heal with confidence
Knowing your wound care plan makes a real difference in how quickly and safely wounds heal — especially chronic wounds. This guide walks you through the essentials: common wound types, advanced treatments, infection prevention, and practical steps patients and caregivers can use every day. By the end, you’ll feel clearer about managing your care and where to find support. Chronic wounds can affect daily life, but with the right guidance and consistent care, you can move through recovery with greater confidence.
Common types of chronic wounds and how they heal
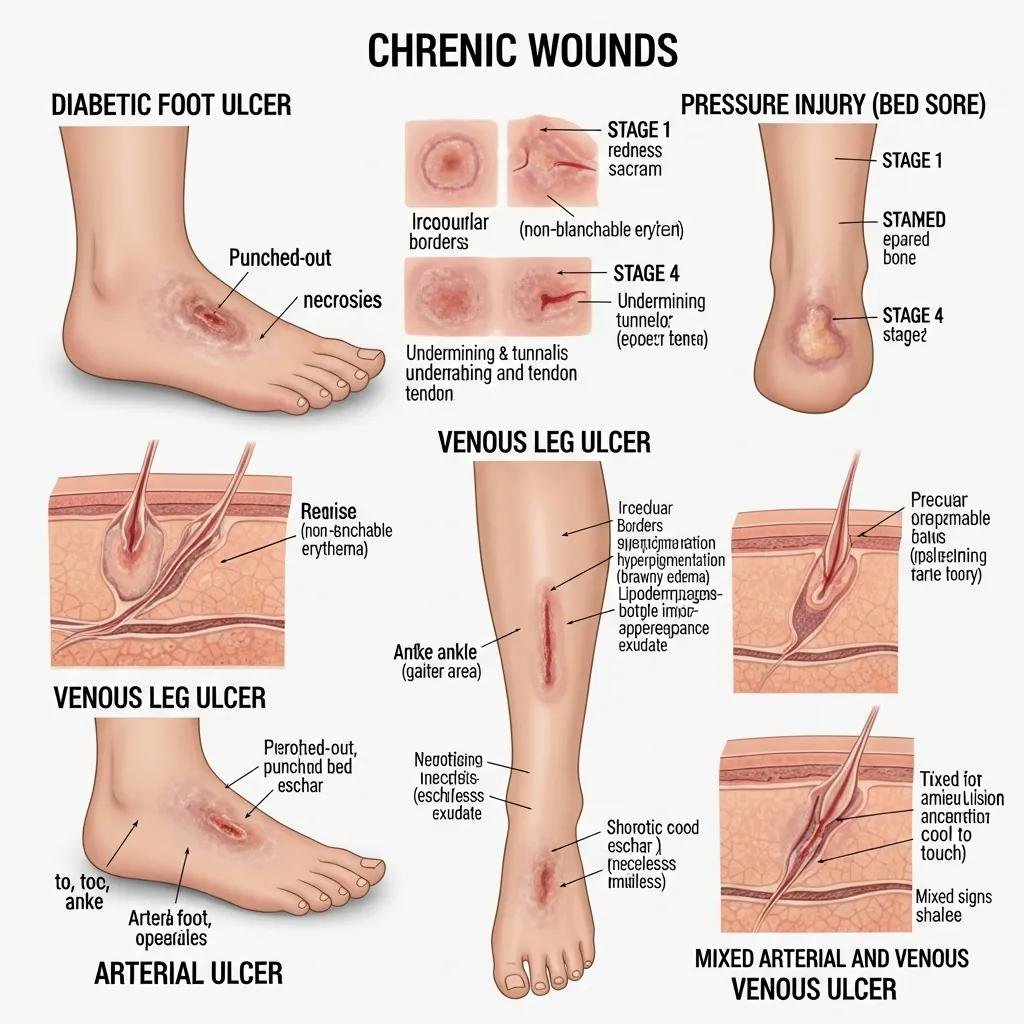
Chronic wounds are wounds that do not heal within the expected time — usually 4 to 6 weeks — often because of underlying health issues. Each type of wound heals differently and needs a tailored approach. Understanding these differences helps you and your care team pick the right treatments.
How diabetic foot ulcers change the healing process
Diabetic foot ulcers often develop when nerve damage (neuropathy) and poor circulation reduce the body’s ability to heal. Less blood flow and a higher infection risk can slow recovery. Managing these wounds means close monitoring, consistent wound care, and controlling blood sugar. Early, targeted intervention can lower the chance of serious complications, including amputation.
What to know about pressure injuries and venous leg ulcers
Pressure injuries (bedsores) form when prolonged pressure cuts off blood flow to the skin, causing tissue damage. Venous leg ulcers result from poor vein function and fluid buildup, which weakens the skin and causes breakdown. Treatment differs: pressure relief and repositioning are key for pressure injuries, while compression and improved circulation help with venous ulcers. Matching treatment to the wound type improves outcomes.
How Healix360’s mobile wound care improves your treatment experience
Healix360
brings specialty wound care to your home so you get personalized treatments without the hassle of travel. Our clinicians deliver evidence-based care in a setting that’s familiar and comfortable, making it easier to stay consistent with your plan.
What happens during a mobile wound care visit?
A certified wound clinician will assess your wound, select and apply the right dressings or therapies, and show you practical steps to support healing at home. The visit usually includes a full wound assessment, dressing changes, and clear guidance on what to watch for as the wound improves. We tailor each visit to your needs so care is practical and focused.
Why advanced wound care at home helps
Receiving advanced care at home adds convenience and comfort while reducing the stress and infection risks of travel. Home visits make it easier for people with mobility limits to get regular care and timely adjustments to treatment. With Healix360’s mobile services, you get high-quality clinical care where you’re most comfortable.
Delivering ongoing wound care at home is practical and can be cost-effective, especially for patients with limited mobility or who live far from clinics.
Benefits of a home-based chronic wound care model
Continuous home wound care, guided by a home-based chronic care model, is a practical alternative that may offer economic and accessibility benefits for people with physical limitations or those in remote locations.
Effectiveness of continuous home wound care on patients with diabetic foot ulcers, 2024
Advanced treatment options for chronic wounds

Treatment for chronic wounds has advanced a lot in recent years. New therapies and technologies help create the right environment for healing. Knowing these options helps you discuss choices with your care team and take an active role in decisions.
How debridement helps wounds heal
Debridement removes dead, damaged, or infected tissue so healthy tissue can grow. It can be done surgically, mechanically, enzymatically, or by using the body’s own processes (autolytic). Clearing non-viable tissue creates a cleaner wound bed, lowers infection risk, and supports faster healing.
Biologic dressings and negative pressure wound therapy: what they do
Biologic dressings — made from natural or bioengineered materials — keep the wound moist and support tissue repair. Negative pressure wound therapy (NPWT) uses controlled suction to remove excess fluid and encourage blood flow. Both approaches can speed healing in many chronic wounds, though results vary by wound type and patient factors.
NPWT has shown meaningful benefits in many cases, but research continues to define when it’s most consistently effective across wound types.
Negative Pressure Wound Therapy and chronic wound healing
Negative Pressure Wound Therapy (NPWT) is an effective tool for supporting chronic wound healing in many situations, though its benefits can vary and warrant ongoing study.
Effectiveness of negative pressure wound therapy on chronic wound healing: A systematic review and meta-analysis, A Burhan, 2022
| Treatment Option | Description | Benefits |
|---|---|---|
| Debridement | Removal of dead or non-viable tissue | Creates a clean wound bed and lowers infection risk |
| Biologic Dressings | Natural or engineered materials that cover the wound | Keeps moisture balance and supports tissue regeneration |
| Negative Pressure Wound Therapy | Controlled suction applied to the wound | Helps remove fluid, reduce swelling, and improve blood flow |
This table highlights key advanced options that can improve healing when used appropriately as part of a comprehensive care plan.
Recognizing and preventing wound infection during your care plan
Spotting infection early and following prevention steps are critical to a successful recovery. Left untreated, infections can slow healing and cause serious complications.
Signs of wound infection to watch for
Look for increasing redness, swelling, warmth, new or worsening pain, or pus-like drainage. Systemic signs such as fever or chills may mean the infection is more serious. Contact your clinician promptly if you notice any of these changes.
Practical strategies to reduce infection risk
Follow your wound care routine: clean the wound as instructed, change dressings when they’re wet or soiled, and avoid touching the wound with unwashed hands. Keep dressings secure and follow any antibiotic or topical treatment guidance your clinician provides. Good hygiene and routine monitoring make a big difference.
Practical steps patients and caregivers can follow for better healing
A structured approach to daily care helps wounds progress. Simple, consistent steps during dressing changes and monitoring give clinicians the information they need to adapt treatment.
How to change dressings and track wound progress
Dressing changes typically follow a clear sequence: wash your hands thoroughly; remove the old dressing carefully; clean the wound with sterile saline or as instructed; then apply the new dressing per your clinician’s directions. Track progress by noting changes in size, drainage, color, and pain — and report concerning signs to your care team right away.
Pain management and nutrition tips to support recovery
Good pain control and proper nutrition support healing. Talk with your clinician about pain relief options, from over-the-counter medicines to prescriptions when needed. A balanced diet with adequate protein, vitamin C, zinc, and other nutrients helps tissue repair. Staying well hydrated is important too.
Where to find support and resources for your wound care journey
Accessing the right resources helps both patients and caregivers manage wound care more confidently. Educational materials, support groups, and trained clinicians are all valuable.
Guidance and training for caregivers
Caregivers are essential partners in wound care. Practical training, clear educational resources, and peer support can boost caregivers’ skills and confidence. Many organizations and clinics offer workshops and online tools to help family caregivers perform basic wound assessments and daily care safely.
Equipping family caregivers with training and resources is key to better wound outcomes and greater caregiver confidence.
Training and support for family caregivers in wound care
Family caregivers benefit from more structured support and training so they can safely perform basic wound assessment and care, including postoperative and chronic wound management.
Teaching wound care to family caregivers: an overview of methods to use to promote wound healing, 2022
How to access Healix360’s patient education and consultations
Healix360 provides patient education and one-on-one consultations to help you and your caregivers feel prepared and supported. Access our materials and
schedule consultations
with wound care specialists who can tailor guidance to your situation. Personalized education helps you stay engaged in care and make informed choices.
Frequently Asked Questions
What should I do if my wound is not healing as expected?
If a wound isn’t improving in the expected timeframe, contact your healthcare provider. They will check for infection, poor circulation, or other issues that can slow healing and may adjust your treatment or recommend advanced therapies. Early evaluation reduces the risk of complications.
How often should I change my wound dressing?
Dressing frequency depends on the wound type and clinician instructions. Change dressings when they become wet or soiled, or as your provider directs. Regular, appropriate changes keep the wound environment clean and support healing.
Can I shower with a wound dressing on?
In many cases you can shower, but protect the dressing so it stays dry. Use a waterproof cover or plastic wrap when needed, and follow your clinician’s specific advice based on dressing type and wound location.
What lifestyle changes support wound healing?
Healthy habits help wounds heal: eat a balanced diet high in protein and nutrients like vitamin C and zinc, stay hydrated, manage chronic conditions (for example, diabetes), avoid smoking, and follow any exercise guidance from your clinician to support circulation.
How can I manage pain related to my wound?
Pain control is part of effective wound care. Discuss options with your clinician — from OTC pain relievers to prescribed medications. Non-drug methods like cold packs and relaxation techniques can also help. Report changes in pain so your care team can adjust treatment.
What should I do if I notice signs of infection?
If you see increased redness, swelling, warmth, pain, or new drainage, contact your healthcare provider promptly. Early treatment — which may include antibiotics or changes to wound care — reduces complications and speeds recovery.
Are there support groups for patients with chronic wounds?
Yes. Support groups and patient organizations offer community, shared advice, and emotional support. Many hospitals and clinics also run support programs. Connecting with others who understand the experience can be very helpful.
Conclusion
A clear wound care plan, consistent care, and the right support make healing more likely and less stressful. Mobile wound care combines clinical expertise with the convenience of home visits, helping you stay on track. Use this guide, lean on your care team, and reach out for personalized support when you need it. Explore Healix360’s services and resources to get the help that fits your recovery plan.







