Chronic Wounds vs Traditional Care: Why Mobile Wound Care Matters
Chronic wounds create ongoing challenges for patients and care teams — they drain energy, delay recovery, and can lead to serious complications. This article breaks down what chronic wounds are, how traditional approaches fall short, and why delivering advanced, personalized wound care in the home can change outcomes. Many people experience slow healing that affects daily life; advanced mobile wound care brings targeted treatments directly to patients to speed healing and reduce risks. Below, we cover wound types, treatment limitations, and the regenerative therapies that are making a real difference.
What Are Chronic Wounds and Why Do They Require Specialized Care?
Chronic wounds are wounds that don’t progress through the normal stages of healing — commonly staying open beyond four weeks or failing to close after three months. They often involve underlying health issues like poor circulation, neuropathy, or infection, so they need focused, ongoing care from clinicians who understand those complexities. Recognizing the wound type and root causes is the first step to effective treatment.
Which Types of Chronic Wounds Are Most Common?
- Diabetic Foot Ulcers: Common in people with diabetes, often driven by nerve damage (neuropathy) and reduced blood flow.
- Venous Leg Ulcers: Caused by poor venous return; these usually show up on the lower legs and need compression and vascular management.
- Pressure Ulcers: Also called bedsores, these form where prolonged pressure limits circulation, especially in immobile or wheelchair-bound patients.
Treating these wounds effectively means addressing both the wound itself and the medical factors preventing healing.
What Complications Arise from Untreated or Poorly Managed Chronic Wounds?
- Infection Risks: Open wounds can become colonized by bacteria, increasing the chance of local or systemic infection.
- Long-term Complications: Without proper care, chronic wounds can lead to cellulitis, osteomyelitis, or in severe cases, amputation.
- Impact on Quality of Life: Ongoing pain, reduced mobility, and emotional strain are common and can significantly lower day-to-day functioning.
Timely, specialized care reduces these risks and supports better long-term outcomes.
How Do Traditional Wound Treatments Compare to Advanced Care?
Traditional wound care — basic dressings, topical medications, and clinic-based follow-ups — can help many acute wounds. Chronic wounds, however, often need a more nuanced approach: advanced therapies, frequent monitoring, and coordinated care that addresses underlying health issues. Understanding those gaps explains why many patients benefit from upgraded treatment pathways.
What Are the Limitations of Traditional Wound Care Methods?
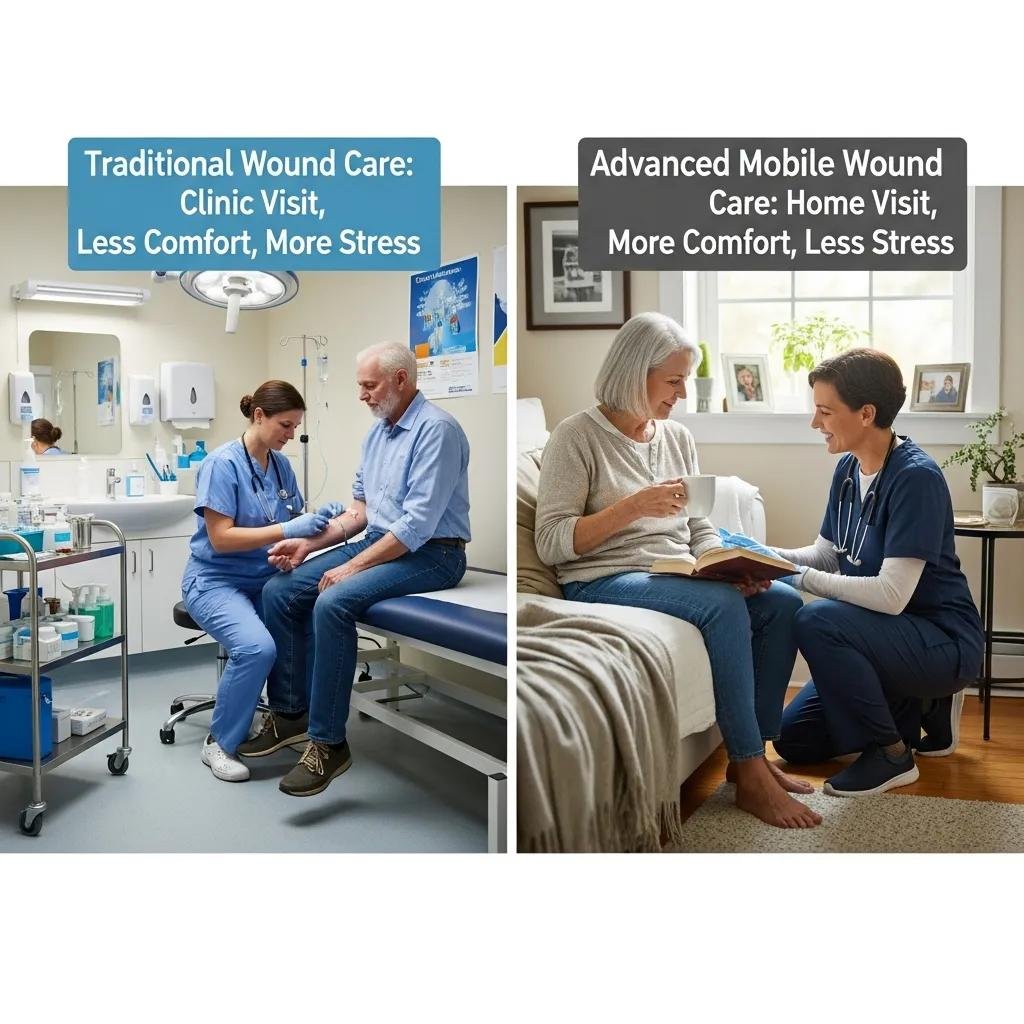
- Frequent Clinic Visits: Repeated trips for dressing changes can be inconvenient, costly, and physically demanding for patients.
- Longer Healing Times: Standard dressings and sporadic follow-up may not provide the biological support or consistency needed for chronic wounds to close.
- Higher Risk of Complications: Less frequent monitoring and one-size-fits-all treatments can allow infections or chronic inflammation to persist.
These limits make clear why some patients need more advanced, tailored care delivered consistently.
Why Do Traditional Treatments Often Result in Slower Healing and Lower Success Rates?
- Lack of Personalized Care: Many conventional approaches don’t adapt to the patient’s overall health, wound environment, or lifestyle.
- Inadequate Treatment Options: Basic therapies may miss opportunities to use regenerative or biologic treatments that accelerate repair.
- Patient Compliance Issues: Complex travel, rigid schedules, and uncomfortable clinic visits can make it hard for patients to stick with a plan.
Addressing those gaps is central to improving healing rates and reducing recurrence.
What Are the Benefits of Advanced Mobile Wound Care for Chronic Wounds?
Advanced mobile wound care combines specialist expertise, evidence-based therapies, and home-based delivery to improve outcomes. Patients get consistent, personalized treatment without the burden of frequent clinic travel — and clinicians can apply advanced tools and close monitoring that speed healing and lower complication rates.
How Does Mobile Wound Care Improve Patient Convenience and Comfort?
- Elimination of Travel Barriers: Care is delivered in the patient’s home, removing transportation challenges and reducing missed appointments.
- Flexible Scheduling: Visits and follow-ups can be arranged around the patient’s life, improving adherence and continuity.
- Familiar Environment for Treatment: Home-based care reduces stress for many patients and supports comfort during longer or more frequent treatments.
These practical advantages help patients stay engaged in their healing plans.
In What Ways Does Advanced Care Accelerate Healing and Reduce Complications?
- Use of Advanced Therapies: Options such as negative pressure wound therapy (NPWT), biologic dressings, and cellular therapies support faster tissue regeneration.
- Regular Monitoring and Adjustments: Ongoing assessments let clinicians tweak treatments quickly when wounds stall or improve.
- Lower Infection Rates: Proactive wound care protocols and timely interventions reduce the chance of infection and related setbacks.
Together, these factors improve both the speed and durability of healing.
Which Regenerative Wound Therapy Options Are Available and How Do They Work?

Regenerative therapies aim to restore healthy tissue by supporting the body’s repair mechanisms. These treatments complement traditional care and can be particularly effective for wounds that have stalled.
What Is Debridement and Why Is It Essential for Healing?
Debridement removes dead, infected, or nonviable tissue from the wound bed to create conditions that support healing. Its benefits include:
- Prevention of Infection: Clearing necrotic tissue reduces bacterial load and the risk of spreading infection.
- Promotion of Healthy Tissue Growth: A clean wound bed encourages granulation and epithelialization.
- Improved Wound Assessment: Debridement exposes the true wound state so clinicians can choose the right next steps.
When performed appropriately, debridement is a foundational step in chronic wound management.
How Do Biologic Dressings, Stem Cell Therapy, and NPWT Promote Tissue Regeneration?
Several regenerative options are commonly used in advanced wound care:
- Biologic Dressings: These deliver growth factors or extracellular matrix components that support cell migration and tissue repair.
- Stem Cell Therapy: Cellular therapies can stimulate repair pathways and improve tissue remodeling in difficult-to-heal wounds.
- Negative Pressure Wound Therapy (NPWT): Controlled suction promotes blood flow, reduces edema, and encourages granulation tissue formation.
Applied thoughtfully, these therapies can shift a chronic wound back into an active healing trajectory.
Ongoing research continues to expand regenerative options and refine how these therapies are used in practice.
Advances in Chronic Wound Healing & Regenerative Medicine
Chronic wounds remain a widespread and costly problem. New regenerative approaches offer promising ways to improve healing and prevent severe outcomes like infection and amputation. Current innovations include customizable matrices made from synthetic and natural polymers; autologous and allogeneic cell therapies at various differentiation stages; small molecules, peptides, proteins and growth factors; as well as RNA interference and gene therapy. Over the past decade, a range of advanced wound dressings and tissue-engineered skin substitutes has emerged to support healing.
Current advances in wound healing and regenerative medicine, M Moradi, 2024
What Can Patients Expect During Their Healing Journey with Advanced Mobile Wound Care?
Patients enrolled in advanced mobile wound care receive a coordinated, individualized program: assessment, tailored therapy, regular follow-up, and education to support recovery at home. Clear communication and measurable goals help set expectations and track progress throughout the healing journey.
How Is a Personalized Treatment Plan Developed and Monitored?
A personalized treatment plan is built from:
- Initial Assessment: A clinician evaluates the wound, circulation, comorbidities, and functional needs.
- Factors Considered: Medical history, medications, nutrition, mobility, and wound characteristics all inform the plan.
- Monitoring Progress: Scheduled visits and remote check-ins allow timely adjustments based on healing milestones or setbacks.
This tailored process helps clinicians apply the right therapies at the right time.
What Role Does Medicare Part B and Insurance Coverage Play in Accessing Care?
Insurance can affect access to advanced mobile wound care in important ways:
- Overview of Medicare Part B: Medicare Part B often covers medically necessary wound care services, including certain home health services when criteria are met.
- Insurance Coverage for Mobile Care: Many private plans and Medicare Advantage policies also cover in-home wound care services — coverage varies by plan.
- Navigating Insurance Claims: Patients and caregivers should work with providers and payers to confirm benefits, prior authorizations, and documentation requirements to avoid surprises.
Discussing coverage early helps make care more predictable and affordable.
How Can Caregivers Support Chronic Wound Management at Home?
Caregivers are critical partners in wound care. Their day-to-day support, observation, and communication with the care team help keep treatment on track and detect problems early.
What Practical Tips Help Caregivers Manage Wound Care Effectively?
- Daily Care Routines: Keep a consistent schedule for dressing changes, wound cleansing, and medication as instructed by the care team.
- Signs of Infection to Watch For: Monitor for increased redness, warmth, swelling, worsening pain, pus, or a bad odor — report these promptly.
- How to Assist with Treatment: Offer emotional support, help with mobility and nutrition, and encourage adherence to appointments and care plans.
Simple, steady routines make a measurable difference in healing.
How Can Caregivers Communicate with Wound Care Specialists for Optimal Support?
- Importance of Clear Communication: Share specific observations, changes in symptoms, and any barriers to following the plan.
- Questions to Ask During Consultations: Ask about expected timelines, warning signs, wound-care techniques, and what to do between visits.
- How to Report Changes in the Wound: Use photos, notes on pain or drainage, and timely phone or portal messages to keep the team informed.
Open, precise communication helps clinicians respond quickly and appropriately.
| Therapy | How it works | Key benefits |
|---|---|---|
| Biologic Dressings | Provide growth factors and structural support to the wound bed | Speeds tissue regeneration and supports cell migration |
| Stem Cell Therapy | Delivers reparative cells or cell signals to promote tissue repair | Enhances healing and tissue remodeling in stalled wounds |
| Negative Pressure Wound Therapy (NPWT) | Applies controlled suction to remove fluid and stimulate blood flow | Improves granulation, reduces edema, and supports closure |
Advanced mobile wound care represents a meaningful shift in how chronic wounds are managed: it pairs specialized therapies with the convenience of home delivery to improve healing, reduce complications, and support patients and caregivers. By understanding wound complexity and the limits of traditional methods, you can choose a care path that prioritizes recovery. If you want to learn more or need help, contact our team.
Frequently Asked Questions
What are the signs that a chronic wound is not healing properly?
Watch for increasing redness, swelling, warmth, persistent or worsening pain, new or increased drainage (especially pus), an expanding wound size, or a foul odor. Any of these signs warrants prompt contact with your wound care team for reassessment.
How can nutrition impact the healing of chronic wounds?
Good nutrition is essential for repair. Adequate protein, vitamins A and C, and minerals like zinc support collagen formation and immune function. A dietitian can help tailor recommendations, especially for patients with diabetes or other conditions that affect healing.
What role do advanced technologies play in mobile wound care?
Tools like telehealth, digital wound imaging, and devices such as NPWT enable remote monitoring, faster adjustments to care plans, and delivery of therapies that previously required clinic visits. Technology helps clinicians stay connected and responsive to patient needs.
How often should chronic wounds be assessed by a healthcare professional?
Assessment frequency depends on wound severity and treatment type but often ranges from weekly to bi-weekly. Patients with high-risk wounds or who are receiving advanced therapies may need more frequent follow-up. Always follow your clinician’s recommended schedule.
What are the potential costs associated with advanced mobile wound care?
Costs vary by treatment, visit frequency, and insurance coverage. Many services are covered by Medicare Part B or private insurance when medically necessary, but out-of-pocket costs can occur. Discuss coverage and billing with your provider early to understand potential expenses and options for assistance.
Can chronic wounds lead to psychological effects, and how can they be addressed?
Yes — chronic wounds can cause anxiety, depression, social isolation, and reduced quality of life. Addressing mental health is a key part of comprehensive care: counseling, support groups, caregiver support, and integrated psychosocial services can all help.
Conclusion
Advanced mobile wound care offers a practical, patient-centered approach to chronic wound management. By combining specialist expertise, regenerative therapies, and in-home delivery, this model improves convenience, accelerates healing, and reduces complications. Caregivers and clinicians working together make recovery more achievable — reach out to our team to learn how mobile wound care can support your healing journey.







