If you’re struggling with a wound that won’t heal, amniotic membrane graft treatment might be the breakthrough you need. These specialized grafts use natural biological materials to jump-start healing in wounds that have resisted every other treatment you’ve tried.
For months, you’ve probably dealt with endless dressing changes, antibiotics, and mounting frustration as your wound stayed stubbornly open. The constant worry about infection, the pain, the limitations on your daily life, it all takes a toll.
But there’s real hope. Amniotic tissue technology represents one of the most exciting advances in wound care, offering a natural solution that works with your body’s own healing mechanisms.
What Is an Amniotic Membrane Graft
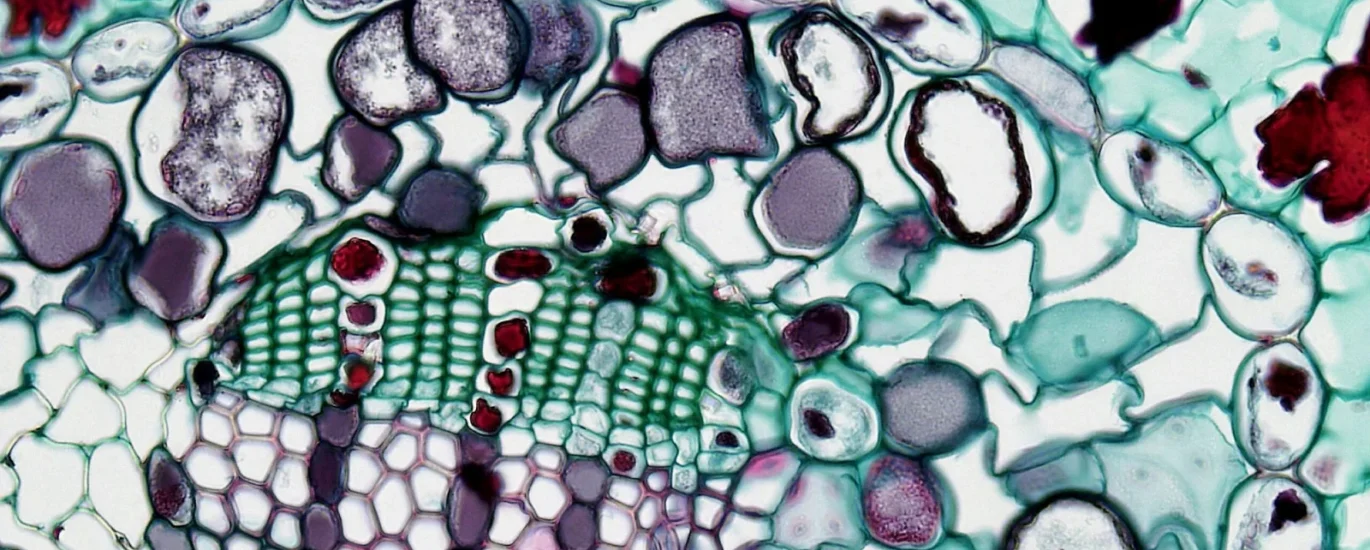
An amniotic membrane graft comes from the innermost layer of the placenta, the tissue that surrounds and protects a baby during pregnancy. After healthy, screened births, this tissue is donated, carefully processed, and preserved for medical use.
Think of it as nature’s wound dressing, but supercharged. The amniotic membrane contains an incredibly rich mix of growth factors, proteins, and other biological substances that promote healing. These are the same factors that help a baby develop and grow, concentrated in a thin, translucent sheet.
The tissue is thoroughly screened for safety, processed to remove cells that could cause immune reactions, and sterilized following strict medical standards. What remains is a biological scaffold packed with healing potential.
When your doctor places an amniotic membrane graft on your wound, it doesn’t just sit there like a regular bandage. It actively participates in the healing process, releasing growth factors and proteins that tell your body to repair itself.
The Science Behind How It Works
The power of amniotic membrane graft technology lies in its biological complexity. This tissue contains over 200 different growth factors and proteins, each playing a specific role in healing.
Epidermal growth factor stimulates skin cells to multiply and migrate across the wound. Transforming growth factor helps reduce inflammation and encourages collagen production. Vascular endothelial growth factor triggers the formation of new blood vessels, bringing oxygen and nutrients to starving tissue.
The membrane also contains hyaluronic acid, which keeps the wound environment moist and creates ideal conditions for cell movement and growth. Plus, it has natural anti-inflammatory properties that calm the excessive inflammation often seen in chronic wounds.
Here’s what makes this so effective. Chronic wounds typically have low levels of growth factors because they’re being destroyed by enzymes in the wound fluid.
The graft provides a physical scaffold too. New cells need something to grow on, a structure to guide their movement. The extracellular matrix in amniotic membrane graft tissue mimics what your body would normally produce, giving cells a roadmap for regeneration.
As healing progresses, your body gradually absorbs the graft while building its own new tissue. The membrane doesn’t need to be removed because it becomes incorporated into the healing process.
Types of Wounds That Respond Well
Amniotic membrane graft treatment works remarkably well for diabetic foot ulcers. These wounds often resist healing because diabetes damages nerves and blood vessels, creating a hostile environment for repair.
Venous leg ulcers, caused by poor circulation in the legs, also respond excellently. The growth factors in the graft help overcome the circulation problems that keep these wounds open for months or years.
Pressure ulcers, the painful sores that develop when someone is bedridden or uses a wheelchair, benefit tremendously from this approach. The tissue provides the biological boost needed to fill in these deep wounds and restore skin integrity.
Surgical wounds that won’t close, traumatic injuries with tissue loss, and burns that struggle to heal all show improved outcomes with amniotic membrane graft applications. Basically, any wound stuck in chronic inflammation rather than active healing is a potential candidate.
What to Expect During Treatment
Getting treated with an amniotic membrane graft starts with a thorough evaluation. Your doctor examines the wound, checks for infection, assesses circulation, and reviews your medical history. They need to make sure you’re a good candidate and that any complications are addressed first.
The actual application is straightforward. First, your doctor cleans the wound thoroughly, removing any dead tissue or debris that could interfere with healing. This debridement step is crucial because the graft needs contact with healthy tissue to work effectively.
Next, they measure your wound and select an appropriately sized graft. The amniotic tissue comes in different sizes and forms, some are sheets, others are particulate or flowable forms that can fill irregular wound shapes.
The doctor places the graft directly onto the wound bed, making sure it covers the entire area with a bit of overlap at the edges. This regenerative approach positions the growth factors exactly where they’re needed most. They then cover it with a standard wound dressing to protect it and keep it moist.
The best part? It doesn’t hurt. Most patients describe the sensation as similar to a regular dressing change. There might be mild pressure or slight discomfort, but nothing like the pain of an infected, open wound.
You’ll need to return for follow-up visits, usually weekly at first. Your doctor checks healing progress and may apply additional grafts if needed. The number of applications varies, some wounds respond to a single graft, while larger or more stubborn wounds might need two to four applications over several weeks.
Timeline for Healing
Most patients start seeing improvements within the first week or two after amniotic membrane graft placement. The wound bed begins to look healthier, inflammation decreases, and you might notice less drainage.
By three to four weeks, new tissue typically fills in the wound base. The edges start moving inward, and the overall size shrinks noticeably. This is when patients often feel hopeful for the first time in months.
Complete closure usually happens between six and twelve weeks, depending on wound size, location, and your overall health. A small diabetic foot ulcer might close in six weeks, while a large pressure ulcer could take three months.
These timelines beat standard care by a significant margin. Wounds that would normally take six months to a year with conventional treatment often heal in half that time with amniotic membrane graft therapy.
Your specific healing speed depends on several factors. Good nutrition, adequate blood flow, controlled blood sugar if you have diabetes, and following your doctor’s instructions all play a role. Patients who optimize these factors see the fastest results.
Supporting Your Body’s Response
While the amniotic membrane graft provides powerful biological support, you need to give your body the raw materials for healing. Protein intake is critical because your body uses amino acids to build new collagen and tissue.
Proper nutrition significantly impacts healing outcomes. Aim for at least 1.2 to 1.5 grams of protein per kilogram of body weight daily. Good sources include lean meats, fish, eggs, dairy, beans, and legumes.
Vitamins and minerals matter too. Vitamin C is essential for collagen synthesis. Zinc supports cell division and immune function. Vitamin A helps with epithelialization, the process of forming new skin. B vitamins provide energy for cellular processes.
If you’re not eating well due to illness or limited appetite, talk with your doctor about nutritional supplements. Sometimes a high-protein shake or multivitamin can make a meaningful difference in healing speed.
Hydration keeps everything running smoothly. Your blood needs adequate volume to deliver nutrients to the wound and carry away waste products. Aim for at least eight glasses of water daily, more if you’re active or it’s hot outside.
Managing underlying health conditions becomes even more important during treatment. If you have diabetes, tight blood sugar control helps the graft work optimally. If circulation is compromised, follow recommendations for compression therapy or medications.

Addressing Safety and Side Effects
One common concern about amniotic membrane graft treatment involves safety. People naturally wonder about using tissue from pregnancy. The screening and processing standards for these grafts are incredibly rigorous.
Donors undergo extensive health screening, more thorough than blood donation requirements. The tissue is tested for infectious diseases and processed in facilities that meet or exceed FDA standards. The end product is safe, sterile, and ready for medical use.
Allergic reactions are extremely rare because the processing removes the cells that could trigger immune responses. What remains is the structural matrix and growth factors, which your body recognizes as compatible.
Most patients experience no side effects at all. A small percentage might have mild, temporary discomfort at the application site. Serious complications are exceptionally uncommon when the treatment is performed by trained healthcare providers.
The graft doesn’t contain live cells from the donor, so there’s no risk of rejection like you’d see with organ transplants. Your body treats the amniotic membrane graft as a healing aid, not as foreign tissue to attack.
Insurance Coverage and Costs
Cost concerns are legitimate, and it’s important to understand the financial side before starting treatment. Amniotic membrane graft therapy is more expensive upfront than standard wound dressings because of the sophisticated biological materials involved.
However, Medicare and most major insurance companies cover these grafts for chronic wounds that haven’t responded to standard care. Coverage typically requires documentation showing you’ve tried conventional treatment for at least four weeks without adequate improvement.
The approval process usually involves your doctor submitting clinical notes, photographs, and treatment history to demonstrate medical necessity. Most claims get approved when properly documented, especially for diabetic foot ulcers and other well-recognized indications.
Even if you have some out-of-pocket costs, consider the bigger picture. These advanced treatments close wounds faster, which means fewer doctor visits, less time off work, and reduced risk of complications like hospitalization or amputation. The total cost of care often ends up lower than months of conventional treatment.
Many wound care clinics have financial counselors who can help you navigate insurance approval and discuss payment options if you have cost-sharing responsibilities. Don’t let financial concerns stop you from asking about this treatment, solutions often exist.
Comparing to Other Wound Treatments
You might wonder how amniotic membrane graft stacks up against other advanced wound therapies. Compared to standard wound care with gauze or foam dressings, the results are dramatically better. Standard dressings protect the wound but don’t actively promote healing at the cellular level.
Negative pressure wound therapy, which uses suction to remove fluid and stimulate healing, can be effective but requires bulky equipment and frequent dressing changes. Amniotic grafts provide continuous growth factor delivery without the hassle of machinery.
Hyperbaric oxygen therapy helps by increasing oxygen delivery to tissues, but it requires multiple sessions in a specialized chamber and doesn’t address growth factor deficiencies. The two can actually work well together, with the oxygen improving the environment for the graft to function.
Synthetic skin substitutes provide a scaffold for healing but lack the rich array of growth factors found in amniotic tissue. They’re useful in some situations but generally don’t match the biological complexity of amniotic membrane graft materials.
Each treatment has its place, and sometimes combining approaches yields the best results. Your doctor can recommend the optimal strategy for your specific wound.
Real Patient Outcomes
The evidence supporting amniotic membrane graft effectiveness is substantial. Clinical studies consistently show higher complete healing rates, faster time to closure, and better quality tissue formation compared to standard care.
In diabetic foot ulcers, healing rates jump from around 30 percent with standard care to 60 to 70 percent with amniotic grafts. That’s a huge difference when you’re talking about saving limbs from amputation.
Venous leg ulcers show similar improvements, with patients finally achieving closure after years of failed treatments. The quality of life improvements are profound, people can walk without pain, return to activities they’d given up, and stop worrying constantly about their wounds.
Pressure ulcers in elderly or immobilized patients heal faster, allowing people to move more comfortably and reducing the risk of serious infections. Families report relief at finally seeing progress after months of decline.
Beyond the statistics, the human impact matters most. Patients describe the emotional burden lifting as they watch their wounds close. The fear of amputation fades. The daily struggle with wound care becomes manageable. Life starts feeling normal again.
Taking the Next Step
If you’re dealing with a wound that won’t heal, don’t wait until complications force desperate measures. The sooner you explore advanced options like amniotic membrane graft therapy, the better your chances of successful healing.
Talk with your doctor about whether you’re a candidate. If they’re not familiar with this treatment, ask for a referral to a wound care specialist who has experience with regenerative therapies. Sometimes getting a second opinion opens doors to options you didn’t know existed.
Come to the appointment prepared. Bring a list of treatments you’ve already tried, medications you’re taking, and questions about what to expect. Understanding the process helps you make informed decisions about your care.
Remember that healing complex wounds often requires a team approach. Your primary doctor, wound care specialist, and sometimes vascular surgeon or diabetes educator all play roles. Don’t hesitate to ask questions or advocate for yourself if you feel like your current treatment isn’t working.
The technology behind amniotic membrane graft treatment has transformed wound care, offering hope where there was frustration and healing where conventional approaches failed. If you’ve been struggling, this might be exactly what you need to finally close that wound and get your life back.
Frequently Asked Questions (FAQs)
1. How many amniotic membrane graft applications will I need?
Most patients need 1 to 4 applications depending on wound size, depth, and healing response. Small wounds often respond to a single graft, while larger or more complex wounds may require multiple applications spaced 1 to 2 weeks apart. Your doctor will monitor progress and adjust the treatment plan accordingly.
2. Does applying an amniotic membrane graft hurt?
No, the application process is generally painless and similar to a regular dressing change. Your doctor will clean the wound first, which might cause brief discomfort, but placing the graft itself feels like gentle pressure. Most patients report the treatment is far less painful than living with an open, chronic wound.
3. How long does an amniotic membrane graft stay on the wound?
The graft stays in place continuously between doctor visits, typically for 1 to 2 weeks. During this time, your body gradually absorbs the membrane while building new tissue. The graft doesn’t need to be removed because it becomes incorporated into the healing wound. Your doctor will assess progress at follow-up visits and apply a new graft if needed.
4. Are there any risks or side effects from amniotic membrane grafts?
Side effects are rare and typically mild. The tissue undergoes rigorous screening and processing to ensure safety, and allergic reactions are extremely uncommon. Some patients may experience temporary mild discomfort at the application site. Serious complications are exceptionally rare when treatment is performed by qualified healthcare providers.
5. Will my insurance cover amniotic membrane graft treatment?
Medicare and most major insurance plans cover amniotic membrane graft therapy for chronic wounds that haven’t healed with standard care after several weeks. Your doctor will need to document previous treatments and demonstrate medical necessity.
Coverage approval rates are high for diabetic foot ulcers, venous ulcers, and pressure ulcers when properly documented.