Quick Links: Navigate Post-Trauma & Complex Wound CarePost-Trauma & Complex Wounds: Why They’re So Hard to Heal—and How to Treat Them
Post-trauma and complex wounds represent some of the most challenging healing situations in wound care. These injuries—from severe accidents, burns, crush injuries, or complications from major surgery—require specialized treatment and often don’t respond to standard care.
Important Definition:
Complex wounds are those with multiple complicating factors—extensive tissue damage, bone exposure, infection, compromised blood supply, or a combination of these issues that prevent normal healing.
What Are Post-Trauma Complex Wounds?
These wounds differ from typical injuries in both severity and healing challenges. They often involve:
- Extensive tissue damage: Multiple layers of skin, muscle, tendon, or bone are affected.
- Compromised blood supply: Damaged blood vessels reduce oxygen and nutrient delivery.
- High infection risk: Contamination from the initial trauma or environment.
- Multiple comorbidities: Conditions like diabetes, smoking, or medications that impair healing.
Common Types of Complex Wounds
Crush Injuries
Result from severe compression forces—such as vehicle accidents, machinery incidents, or falls. These injuries cause widespread tissue damage beneath the skin, including muscle death, compartment syndrome, and vascular injury.
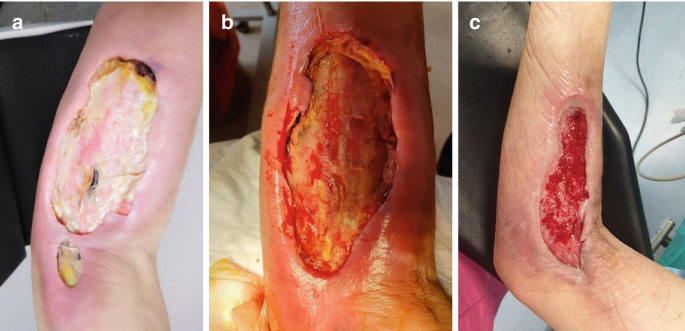
Degloving Injuries
Occur when skin and underlying tissue are torn away from the body. The remaining tissue often has severely compromised blood supply, making healing extremely difficult.
Severe Burns (2nd & 3rd Degree)
Deep thermal injuries that destroy multiple layers of skin and underlying structures. They carry high risk of infection, fluid loss, and significant scarring, and often require grafting.
Open Fractures with Soft Tissue Loss
Broken bones that pierce through the skin and are combined with significant soft tissue loss. Exposed bone is extremely vulnerable to infection (osteomyelitis) and delays wound closure.
Failed Surgical Flaps or Grafts
When reconstructive surgery fails—meaning transplanted tissue dies because of inadequate blood supply. This leaves a complex wound that’s even harder to treat than the original defect.
Necrotizing Fasciitis
A rapidly spreading bacterial infection that destroys tissue layers. Emergency surgical debridement is required, leaving large, complex wounds that must then heal by secondary intention or advanced reconstruction.
Why These Wounds Are So Difficult to Heal
Multiple factors work against the normal healing process:
Vascular Damage
Injured blood vessels can’t deliver enough oxygen and nutrients. Without adequate circulation, tissue regeneration is severely limited.
Biofilm Formation
Bacteria can form protective biofilms that resist antibiotics and immune response, leading to persistent, low-grade infection.
Chronic Inflammation
Instead of moving through normal healing phases, the wound becomes stuck in the inflammatory stage, blocking tissue rebuilding.
Tissue Necrosis
Dead tissue must be completely removed before healing can begin. This often requires repeated debridement procedures.
The Complex Wound Treatment Approach
Treating complex wounds requires a multi-modal strategy that addresses all underlying complications:
1. Aggressive Infection Control
Wound cultures identify specific bacteria. Targeted oral or IV antibiotics, antimicrobial dressings, and sometimes hyperbaric oxygen therapy are used to eradicate infection.
2. Surgical Debridement
All dead, infected, or non-viable tissue must be removed. Multiple debridements may be needed to achieve a healthy wound bed ready for regeneration.
3. Vascular Assessment & Improvement
Blood flow is evaluated with imaging studies. Vascular surgery or interventional procedures may be required to restore circulation before healing can progress.
4. Negative Pressure Wound Therapy (NPWT)
Vacuum-assisted closure helps reduce edema, promote granulation tissue formation, and prepare the wound bed for closure or grafting.
5. Advanced Regenerative Therapies
Once infection is controlled and blood flow improved, advanced biologics such as stem cells, amniotic membrane grafts, and bioengineered skin substitutes can significantly accelerate healing.
Regenerative Options for Complex Wounds
Several advanced biologic therapies are transforming outcomes for complex wounds:
Stem Cell Therapy
Promotes angiogenesis (new blood vessel formation) and supports cellular regeneration in tissue with compromised blood flow. Especially helpful for wounds that have stalled despite standard treatment.
Amniotic Membrane Allografts
Provide growth factors, reduce inflammation, and serve as a natural protective barrier. Particularly effective for large surface wounds and exposed structures.
Dermal Scaffolds
Collagen-based matrices that provide a framework for new tissue ingrowth. Often used as a bridge before skin grafting or in areas too large or complex for simple closure.
Platelet-Rich Plasma (PRP)
Concentrated growth factors from the patient’s own blood. PRP stimulates cellular proliferation, collagen production, and tissue regeneration.
Expected Timeline for Complex Wound Healing
Healing complex wounds is a marathon, not a sprint. Realistic expectations help patients and families stay encouraged:
Weeks 1–4: Stabilization Phase
Focus on controlling infection, removing dead tissue, and establishing a clean, stable wound bed. Visible progress may be slow, but this foundation is critical.
Weeks 5–12: Active Healing Phase
Granulation tissue forms, the wound begins to contract, and regenerative therapies are applied. Week-by-week improvement becomes more noticeable.
Months 3–6+ : Closure & Remodeling
The wound closes through secondary intention or requires surgical closure/grafting. Scar maturation and remodeling continue for up to 1–2 years.
Patient & Caregiver Support
Complex wounds affect far more than just the injured area—they impact entire lives. Supportive care is essential:
- Dedicated wound care team: Specialized nurses and physicians coordinating advanced treatment.
- Nutritional support: High-protein, nutrient-dense diet is often required—sometimes with supplements.
- Pain management: Adequate pain control improves mobility, sleep, and overall healing.
- Mental health support: Long recovery periods can be emotionally draining; counseling or support groups may help.
The Bottom Line
Complex post-trauma wounds are challenging—but they are healable with the right expertise and treatment plan. A multidisciplinary team using advanced regenerative therapies can achieve closure even in the most difficult cases. Early intervention with specialized care dramatically improves outcomes and quality of life.
Dealing with a Complex Wound?
Get connected with specialists who have experience treating the most challenging wounds.