The future of mobile wound care: advances, patient benefits, and emerging therapies
Mobile wound care is changing how chronic and hard‑to‑heal wounds are treated. By bringing advanced therapies and specialist expertise directly into homes, assisted living, and skilled nursing settings, clinicians can deliver tailored care where patients feel safest. Below we outline the latest technologies, patient benefits, and regenerative treatments shaping this shift — including the practical approach used by Healix360 Specialists.
What recent advances are changing home‑based wound treatment?
New tools and workflows are improving outcomes for patients treated outside the clinic. Innovations such as sensor‑enabled dressings and continuous remote monitoring give clinicians actionable data. Meanwhile, telehealth platforms connect patients and specialists quickly for timely assessment and care adjustments. Together, these advances make home treatment more precise, proactive, and convenient.
How do smart dressings and remote monitoring improve healing?
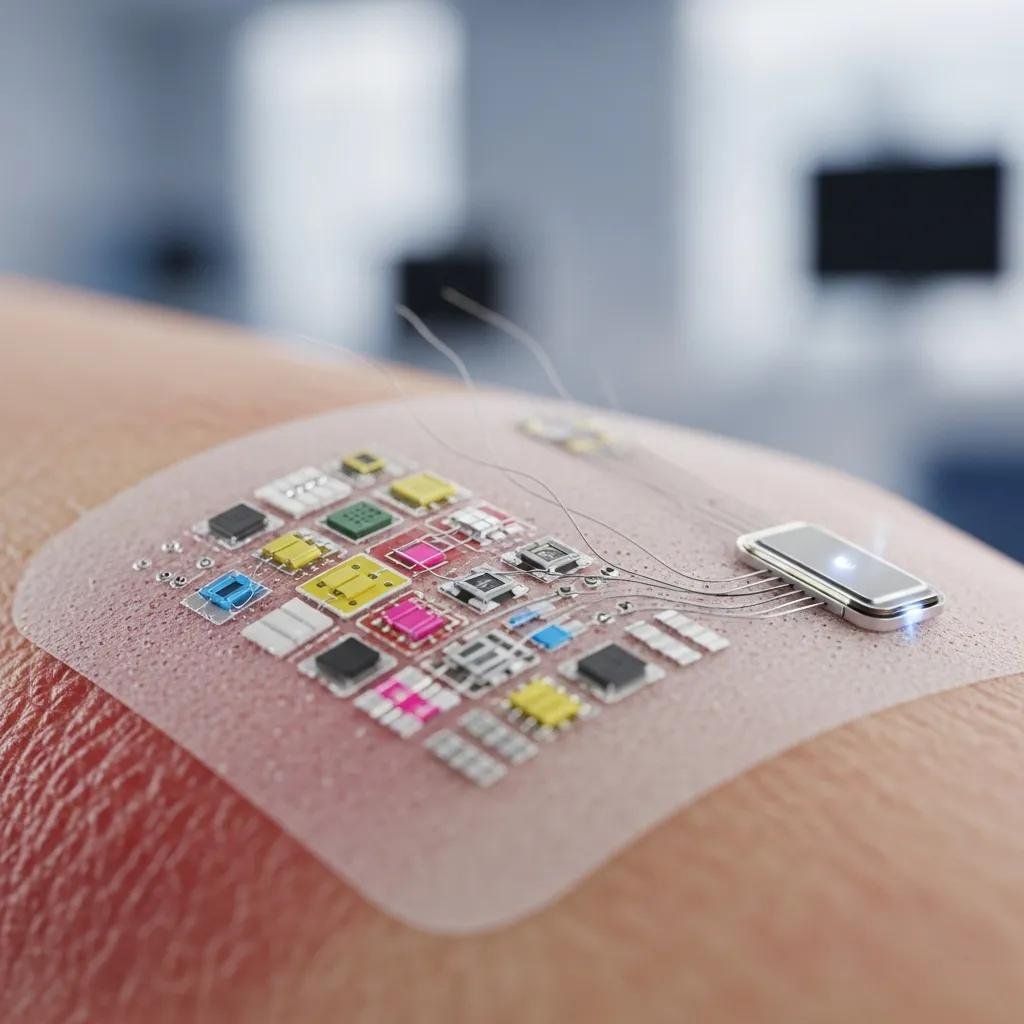
Smart dressings use embedded sensors to track wound conditions like moisture, temperature, and pH. That data helps clinicians detect trouble early and fine‑tune dressings or therapies without waiting for the next in‑person visit. Remote monitoring supports continuous evaluation, reduces unnecessary travel, and focuses clinic time on patients who need hands‑on intervention.
What role do telehealth platforms play in mobile wound care?

Telehealth connects patients and wound specialists for virtual assessments, treatment reviews, and education. It increases access for people with limited mobility or who live far from specialty clinics. Used alongside in‑home visits and remote monitoring, telehealth helps keep care continuous and responsive.
Telemedicine offers clear practical advantages, though research has shown mixed results on its impact for chronic wounds.
Telemedicine for Chronic Wound Management
Background: Chronic wounds place a heavy burden on patients and health systems. Widespread access to the internet and smart devices has made telemedicine an attractive option to support wound care. However, published studies report inconsistent findings about how much telemedicine alone improves long‑term wound outcomes.
Telemedicine in chronic wound management: systematic review and meta-analysis, 2020
How are advanced regenerative wound therapies delivered at home?
Regenerative approaches — from bioengineered skin substitutes to platelet‑rich plasma (PRP) — are increasingly integrated into home care when appropriate. These biologic treatments aim to jump‑start healing in wounds that have stalled with standard care. While many stem cell therapies remain investigational, several regenerative products are now feasible to administer in a home setting by trained specialists, improving convenience and outcomes for complex cases.
What are stem cell and biologic therapies in mobile wound care?
Biologic therapies use naturally derived elements — growth factors, engineered tissues, or PRP — to promote repair and reduce chronic inflammation. Stem cell approaches show promise but are mainly in clinical trials and aren’t yet routine for mobile care. When indicated, biologic treatments can be delivered safely at home, expanding options for patients who would otherwise need clinic‑based procedures.
Regenerative medicine continues to expand the toolkit for difficult wounds, opening new patient‑centered possibilities.
Regenerative Medicine: Future Wound Care Therapies
Recent advances in regenerative medicine and tissue engineering point to more patient‑specific solutions. Mesenchymal stem cells (MSCs) and their secretions have shown particular promise, and technologies such as tissue nano‑transfection enable targeted, in‑place gene modulation without extensive lab work. Methods like 3D bioprinting and extracellular matrix (ECM) bioscaffolds address wounds at cellular and molecular levels, aiming to reduce harmful inflammation and reactivate natural repair pathways.
Emerging technologies in regenerative medicine: The future of wound care and therapy, S Ghatak, 2024
How do growth factors and advanced debridement techniques support healing?
Growth factors trigger cellular processes essential for tissue repair, while modern debridement removes nonviable tissue to create a cleaner wound bed. Combined, these strategies help reestablish the biological conditions needed for healing and can shorten recovery time when applied as part of a coordinated care plan.
What benefits do patients see from advanced mobile wound care?
Receiving advanced wound care at home generally improves comfort, reduces disruption, and enables earlier intervention for complications. Patients often benefit from better pain control, more consistent infection management, and higher satisfaction because care is delivered in a familiar environment and tailored to their needs.
How does in‑home wound treatment improve comfort and safety?
Home‑based treatment reduces the stress and logistical burden of clinic visits. Patients are treated where they live, which can ease anxiety and support better adherence to follow‑up plans. Clinicians can also observe environmental factors that affect healing and adapt care plans to each person’s daily routine.
Studies of integrated home‑to‑hospital support models emphasize the potential clinical benefits of coordinated care.
Home Care Wound Support Network Efficacy
This study evaluated a wound support network linking primary home care services with hospital specialists. Results showed improved clinical outcomes when specialist oversight and clear care pathways were available at home. The findings also highlight that specialized wound expertise is not uniformly available across all primary care services.
Improved clinical efficacy with wound support network between hospital and home care service, 2016
How are pain and infection managed effectively at home?
Effective in‑home management combines appropriate dressings, targeted topical treatments, timely antibiotics when needed, and patient education. Clinicians also teach caregivers how to recognize warning signs and perform simple, evidence‑based care tasks so infections and pain are addressed before they worsen.
How does Healix360 shape the future of mobile wound care services?
Healix360 Advanced Mobile Wound Care Specialists focuses on bringing specialist, regenerative‑aware care to patients where they live. We combine proven clinical protocols, on‑site assessment, and technology‑enabled monitoring to deliver individualized plans that aim for faster, safer healing.
What is Healix360’s unique approach to advanced mobile wound care?
Our model centers on individualized care plans developed by wound specialists. We integrate advanced dressings, regenerative options when appropriate, telehealth follow‑up, and caregiver education to keep care coordinated and responsive. The goal is measurable improvement with less disruption to the patient’s life.
What success stories and clinical outcomes demonstrate effectiveness?
Clinical outcomes and patient reports show meaningful reductions in wound size, fewer complications, and higher satisfaction when care is delivered by experienced mobile wound teams using targeted therapies. Healix360’s combined use of technology and specialist skills supports these positive results for many patients with chronic or complex wounds.
How are caregivers supported in managing chronic wounds at home?
Caregivers are an essential part of long‑term wound management. Mobile wound care teams provide training, clear care plans, and direct access to clinicians so caregivers feel confident and supported when managing dressings, monitoring progress, and escalating concerns.
What resources and communication strategies assist caregivers?
We offer simple, practical education materials, scheduled check‑ins, and secure communication channels to answer questions and adjust care plans. Clear instructions and timely support reduce caregiver uncertainty and improve adherence to treatment regimens.
How can long‑term wound management prevent complications?
Proactive long‑term management — regular assessment, timely debridement, appropriate dressing selection, and early infection control — prevents common complications. Training caregivers to spot early warning signs and keeping clinicians involved through remote monitoring or visits helps protect patients from setbacks.
| Treatment | What it is | Patient benefits |
|---|---|---|
| Smart Dressings | Dressings with sensors to track wound conditions | Real‑time data that supports targeted care |
| Telehealth Platforms | Virtual visits and remote specialist support | Faster access to guidance and fewer unnecessary trips |
| Regenerative Therapies | Biologic options such as bioengineered skin substitutes and platelet‑rich plasma | Enhanced healing potential for chronic wounds |
These modalities, when combined in a coordinated mobile care program, expand options for patients and contribute to better clinical outcomes and quality of life.
Mobile wound care is reshaping how chronic wounds are treated. With advances in technology and biologic therapies, patients can access high‑quality, specialist care at home. As practice evolves, the emphasis on patient‑centered, evidence‑based strategies will continue to improve healing and daily living for people with complex wound needs.
Frequently asked questions
Who benefits most from mobile wound care services?
Patients with chronic wounds — for example, diabetic foot ulcers, pressure injuries, and venous leg ulcers — often benefit most. Mobile care also helps people with limited mobility, those in remote areas, and anyone who prefers coordinated care at home. Personalized, specialist‑led plans improve engagement and outcomes for these groups.
How do mobile wound care services maintain high quality?
Quality comes from trained clinicians, evidence‑based protocols, and technology that supports decision‑making. Specialists in wound care receive targeted training and use tools like smart dressings and telehealth to monitor progress. Regular follow‑ups and patient feedback ensure plans are adapted as healing progresses.
What challenges do mobile wound care programs face?
Common challenges include travel logistics, scheduling in dispersed communities, variable access to advanced tools, and inconsistent insurance coverage. Overcoming these barriers requires operational planning, partnerships with local providers, and advocacy to expand reimbursement for mobile models.
How should patients prepare for a mobile wound care visit?
Prepare a clean, well‑lit area with easy access to the wound site. Have a list of medications, relevant medical records, and notes about recent changes in the wound or symptoms. Clear, open communication helps the clinician tailor the visit and the ongoing care plan.
What role does technology play in mobile wound care?
Technology improves monitoring, communication, and documentation. Sensor dressings provide objective wound data, telehealth enables timely specialist input, and electronic health records keep care coordinated across providers. Together, these tools make treatment more efficient and safer.
Will insurance cover mobile wound care services?
Coverage varies by insurer, plan, and the services provided. Medicare, Medicaid, and many private plans may cover aspects of home health and wound management when medically necessary. Patients should check specific benefits and any out‑of‑pocket responsibilities with their insurer.
Conclusion
Mobile wound care brings advanced, specialist treatment into the places patients call home — improving comfort, access, and often clinical results. Innovations like smart dressings, telehealth, and regenerative options expand what’s possible outside the clinic. If you or a loved one are managing a chronic wound, Healix360 can help design a personalized plan that fits your needs and life. Explore our services to learn how we support safer, faster healing at home.







