Telemedicine Tools for Mobile Wound Care: Virtual Monitoring & Imaging
Telemedicine is reshaping how wound care reaches people — especially those who can’t easily get to a clinic. Using secure video, mobile apps and digital imaging, remote care lets specialists monitor wounds, guide treatment and make timely decisions without repeated in-person visits. This piece explains how telemedicine works in mobile wound care, the technologies that make it possible, and the practical benefits for patients with chronic wounds. Many people with long‑standing wounds struggle to access specialist care, which can delay healing and raise complication risk. Virtual care helps by connecting patients and carers with wound clinicians quickly, improving outcomes and comfort. Below we outline the advantages of telehealth for chronic wounds, the assessment tools clinicians use, and how patients and caregivers can engage effectively with remote services.
Studies underscore the heavy burden of chronic wounds and show how virtual care models are being tested to improve access — especially for people in vulnerable or remote communities.
Virtual Wound Care Interventions for Chronic Wounds
Background: Chronic wounds — those that fail to progress through normal healing — create substantial health and economic strain. Older adults, particularly residents of nursing homes, are often most affected. Effective prevention and treatment improve outcomes but are limited by workforce shortages, fragmented services and scarce local specialist access in rural and residential aged care settings. Virtual wound care solutions, such as WoundView (Coviu Global Pty Ltd), use computer-vision and other digital tools to support remote assessment and clinician decision-making.
Virtual Wound Care in Australian Nursing Homes: Protocol for a Pilot and Feasibility Study, A Banbury, 2025
What Is Telemedicine for Wound Healing and How Does It Work?
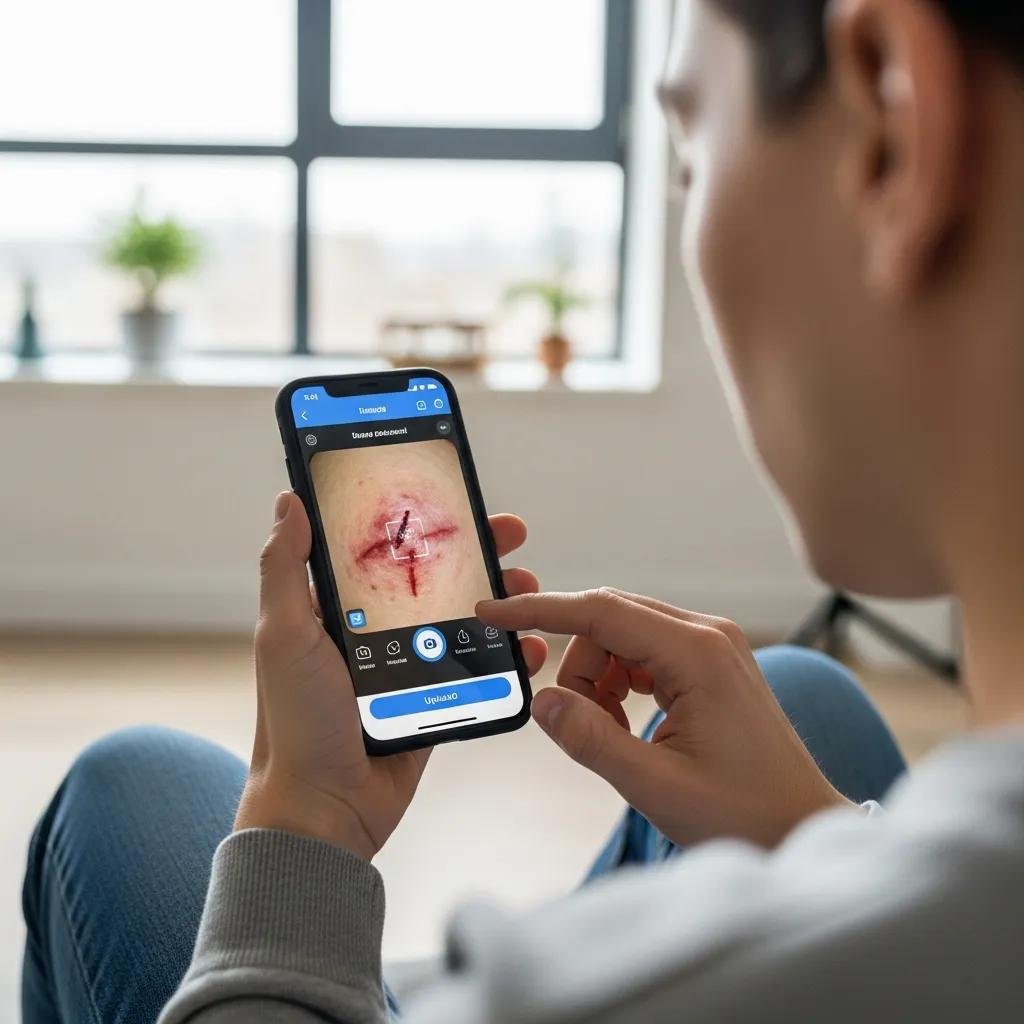
Telemedicine for wound healing uses digital communications to deliver remote assessment, monitoring and treatment guidance. Clinicians can evaluate wounds via secure video, review high-quality photos or use purpose-built apps to track progress. This model helps providers triage needs, adjust dressings or therapies, and escalate care when necessary — all while reducing travel and appointment burden for patients. The main advantage is timely specialist input delivered where the patient is most comfortable: at home or in residential care.
Widespread use of smartphones, tablets and secure telehealth platforms has made remote wound management more practical and reliable for routine follow-up and specialist review.
Telemedicine for Chronic Wound Management: A Review
Background: Chronic wounds place a continual burden on patients and health systems. The widespread availability of internet-connected devices — smartphones and tablets — has enabled telemedicine (TM) approaches to support wound management, offering new pathways to monitor and treat chronic wounds remotely.
Telemedicine in chronic wound management: systematic review and meta-analysis, 2020
How Virtual Wound Care Platforms Enable Remote Patient Monitoring
Virtual wound-care platforms let clinicians follow healing trajectories between visits. Typical features include secure messaging, on-demand video consults and image upload for visual assessment. These tools keep patients engaged with their care plan, support adherence to dressing and offloading instructions, and give clinicians a clearer picture of progress so they can make timely adjustments.
What Mobile Wound Care Technologies Support Telehealth Services?
A range of mobile technologies underpins telehealth wound care: high-resolution imaging devices and smartphone cameras for accurate photos, apps that capture symptom reports and track wound metrics, and wearables that monitor vital signs or mobility. Together these data help clinicians detect complications early and coordinate interventions without always requiring in-person visits.
Emerging tools — including AI-assisted image analysis and automated measurement — are improving the consistency and speed of remote wound assessments.
AI-Powered Telemedicine Device for Wound Monitoring
The Wound Viewer (WV) is an example of a device that captures lesion images and applies an integrated AI algorithm to detect and segment the wound area, then provide measurements and classification information such as estimated area and depth to support clinical decision-making.
Development and Implementation of a Telemedicine System for Wound Care in Different UE Environments., R Cavazzana, 2024
What Are the Benefits of Telehealth Wound Management for Chronic Wounds?
Telehealth wound management delivers clear benefits for people with chronic wounds: it brings specialist oversight sooner, lowers care costs, and broadens access to services that might not exist locally. Remote care complements in-person treatment and can reduce complications when used appropriately.
- Improved Patient Outcomes
: Faster specialist input and regular visual reviews help prevent avoidable complications and support steady healing. - Cost-Effectiveness
: Fewer in-person visits mean reduced travel, less time away from daily life and lower system costs. - Increased Access to Care
: Telehealth connects patients in rural, regional or underserved areas with wound care expertise they might otherwise lack.
For example,
Healix360
Advanced Mobile Wound Care Specialists demonstrate how remote care can improve safety, comfort and outcomes for people managing chronic wounds.
How Does Telemedicine Improve Patient Outcomes and Comfort?
Telemedicine supports better outcomes by enabling regular checks, early treatment changes and direct clinician feedback. Patients benefit from reassurance, faster problem resolution and fewer stressful clinic trips — all of which support comfort and adherence to therapy.
In What Ways Does Telehealth Reduce Healthcare Costs and Increase Access?
Telehealth reduces costs by cutting the need for routine face-to-face appointments and associated travel. It also opens specialist care to patients who live far from services or have mobility or transport barriers, ensuring more equitable access to wound expertise.
Which Remote Wound Assessment Tools and Methods Are Used in Telemedicine?
Accurate remote assessment relies on specific tools and methods so clinicians can make safe decisions without a hands-on exam. These include standardized photo protocols, validated measurement tools, and secure platforms for sharing images and clinical notes.
How Are Digital Wound Imaging and Secure Telehealth Platforms Utilized?
Clinicians use digital imaging to document wound appearance and progression; images and notes are transmitted over secure telehealth platforms that protect patient data while enabling timely specialist review. Consistent image technique and high-quality photos are essential for reliable remote assessment.
What Are the Telehealth Wound Management Guidelines for Remote Assessments?
Guidelines focus on accurate image capture, reliable symptom reporting and strong communication channels. Key practices include using good lighting, consistent photo angles, secure data handling and clear escalation pathways when wounds show signs of deterioration.
How Does Telemedicine Support Caregivers in Mobile Wound Care?

Telemedicine strengthens the role of caregivers by giving them direct access to clinicians, practical guidance and educational resources. That support helps caregivers feel confident in day‑to‑day wound tasks and in recognising when to seek urgent help.
What Resources and Communication Channels Are Available for Caregivers?
Caregivers can use telehealth platforms to access step-by-step care guides, secure messaging with clinicians, video demonstrations and community or peer support where available. These channels reduce uncertainty and build practical skills for safe wound management at home.
How Do Remote Treatment Plans Facilitate Caregiver Involvement?
Remote treatment plans give caregivers clear, timely instructions and scheduled follow-ups so they can carry out dressings, offloading and monitoring with clinician oversight. Regular updates and easy access to the care team keep everyone aligned and responsive to change.
Which Wound Types Are Effectively Treated via Telemedicine?
Telemedicine works well for many chronic and non‑healing wounds that need specialist input but not constant hands-on procedures. It’s a useful adjunct to in-person care for a range of wound types when used with appropriate safeguards.
Can Diabetic Foot Ulcers Be Managed Through Virtual Wound Care?
Diabetic foot ulcers are a frequent and serious issue for people with diabetes. Virtual care supports close monitoring, education on foot protection and timely changes to treatment — reducing the risk of complications when combined with in-person review where needed.
How Are Pressure Injuries and Venous Leg Ulcers Assessed Remotely?
Pressure injuries and venous leg ulcers can be assessed with high-quality photos, symptom reports and recorded progress metrics. Clinicians use these data to recommend care steps, adjust dressings or refer for in-person intervention if the wound is not responding.
How Can Patients Schedule and Prepare for Virtual Wound Care Appointments?
Booking and preparing for a virtual visit is simple and helps make the consultation effective. Good preparation increases the value of remote reviews and supports continuity of care.
What Is the Initial Consultation Process for Telemedicine Wound Care?
In the first consultation patients provide wound history, previous treatments and relevant medical background. Clinicians may ask for current photos and discuss overall health to create a personalised plan and arrange follow-up.
How Are Weekly Follow-ups Structured in Remote Wound Monitoring?
Weekly remote follow-ups typically include updated photos, symptom check-ins and brief video or messaging reviews. These touchpoints allow clinicians to track progress, tweak treatment and escalate care if healing stalls.
Frequently Asked Questions
What types of healthcare professionals are involved in telemedicine for wound care?
Telemedicine for wound care usually involves a multidisciplinary team: wound care specialists, registered nurses, podiatrists and primary care clinicians. They work together via secure digital tools to assess wounds, share findings and coordinate treatment so patients receive comprehensive, team-based care.
How can patients ensure their privacy during telemedicine consultations?
To protect privacy, choose telehealth platforms that follow applicable regulations and use encryption. Conduct consultations in a private space, confirm the platform’s privacy practices and avoid sharing sensitive data in unsecured channels. Your provider should explain how your health information is stored and shared.
What challenges might patients face when using telemedicine for wound care?
Common challenges include limited access to devices or reliable internet, difficulty capturing clear images, and unfamiliarity with digital tools — especially among older adults. Physical examination limits can also complicate some assessments. These issues are often addressed with simple training, caregiver support and hybrid care models that combine virtual and in-person visits.
Are there specific guidelines for patients to follow during virtual wound assessments?
Yes. Patients should prepare high-quality photos (good light, consistent angles), describe symptoms clearly, and have recent treatment details available. Follow clinician instructions for dressing changes and reporting concerns. These steps help clinicians make informed remote decisions.
How does telemedicine address the needs of patients in rural areas?
Telemedicine opens specialist access to people in rural and remote locations by removing distance as a barrier. Virtual consultations reduce travel time and cost and enable timely specialist advice that can prevent deterioration and reduce the need for long-distance transfers.
What role does patient education play in telemedicine for wound care?
Education is central to telemedicine: clinicians deliver practical advice on wound care techniques, hygiene, signs of infection and when to seek urgent help. Empowering patients with knowledge improves adherence, self-monitoring and healing outcomes — especially when paired with clear follow-up plans.
Conclusion
Telemedicine is changing how wound care is delivered by making specialist input more accessible, timely and convenient. When combined with good imaging practices, secure platforms and clear care pathways, remote monitoring can reduce visits, lower costs and support better healing. If you or someone you care for has a chronic wound, explore telemedicine options to see how remote support can fit into a safe, personalised care plan.







