When Chronic Wounds Fail to Heal: Signs You Need Advanced Care
A chronic wound is one that does not move through the normal stages of repair within an expected timeframe—commonly four to twelve weeks. Fixing it means finding the specific reasons healing has stalled. This guide explains why wounds become chronic, the clinical signs that show healing has stopped, and practical thresholds for when to involve specialists. You’ll learn how poor circulation, diabetes, persistent infection and biofilm, pressure, nutrition, and certain medications interfere with repair and what clinicians measure to decide next steps. We outline assessment methods, referral timelines, and modern treatments that speed recovery—like regenerative options and negative pressure wound therapy—plus how in‑home advanced care makes these therapies more accessible. Throughout, clinical and patient-centered language ties together terms such as chronic wound care, diabetic ulcer treatment, wound debridement types, regenerative medicine for wounds, and Medicare wound care benefits.
What Are Chronic Wounds and How Do They Differ from Normal Wounds?
Chronic wounds stay stuck in a prolonged inflammatory phase instead of progressing through the normal sequence—hemostasis, inflammation, proliferation, and remodeling—so the tissue fails to close. Acute wounds usually shrink and fill with healthy granulation tissue over days to weeks; chronic wounds often show persistent drainage, fragile tissue, or little to no healthy granulation. Recognizing this difference matters because basic care—cleaning and simple dressings—often won’t fix the root problem. Early identification of a wound as chronic shifts the team’s focus from surface care to correcting underlying barriers, which improves the chance of durable healing.
What Types of Chronic Wounds Require Advanced Care?
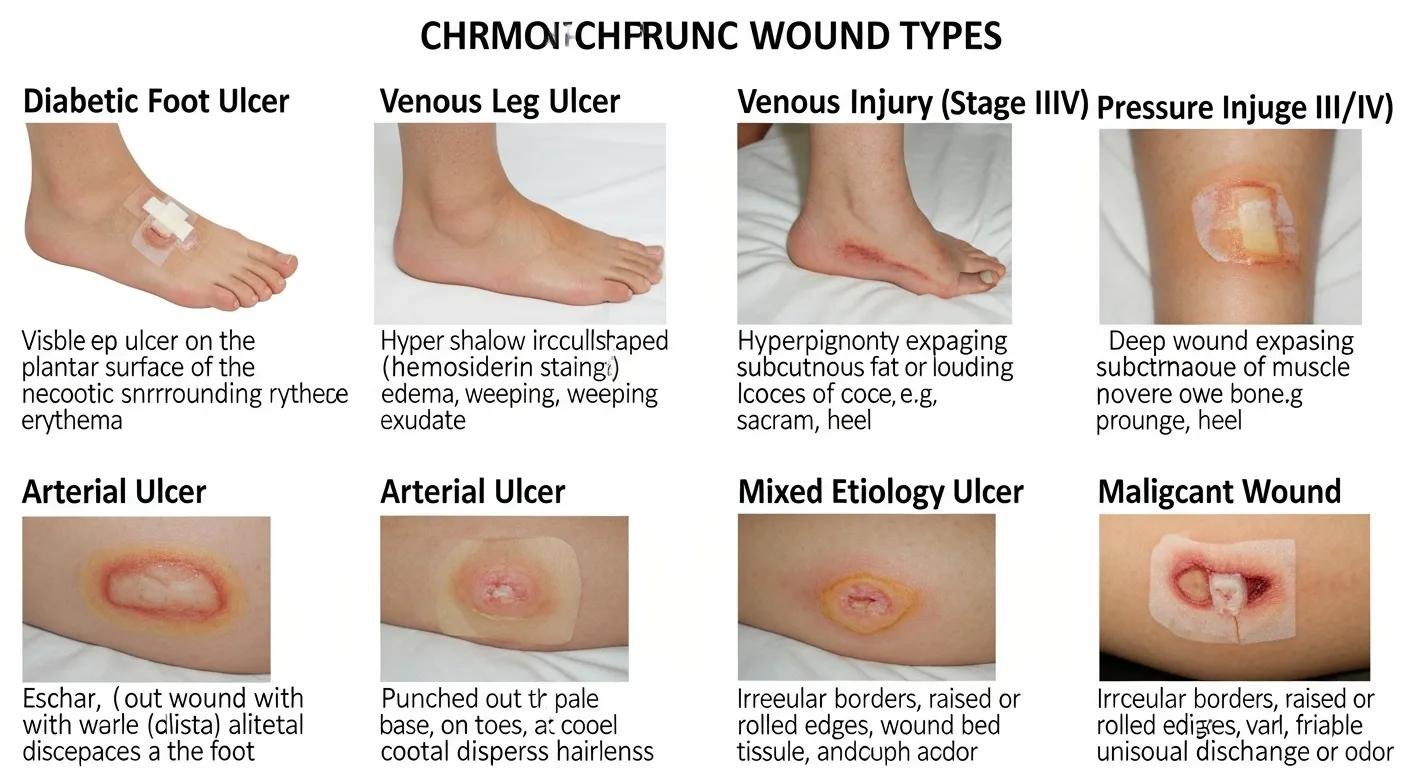
Certain wounds commonly become chronic and often need specialist intervention because they carry higher risk of complications or poor spontaneous healing. Diabetic foot ulcers may progress due to neuropathy and impaired microvascular flow, letting small injuries worsen or become infected. Venous leg ulcers are driven by venous hypertension and edema that prevent closure. Pressure ulcers arise from prolonged loading and shear in immobile patients. Arterial and ischemic ulcers reflect poor perfusion and typically require vascular assessment, and complex post‑surgical or burn wounds may need grafts or advanced biologic dressings. Each wound type brings specific risks—such as infection, osteomyelitis, or limb loss in diabetic foot ulcers—so timely specialist evaluation is often indicated.
How Is a Chronic Wound Diagnosed and When Is It Considered Non-Healing?
Diagnosis blends history, physical exam, and objective tests to find why a wound isn’t progressing and when to label it non‑healing. Clinicians record wound size, depth, wound‑bed tissue types, and drainage, using photos and serial measurements to track change. Typical steps when healing stalls include vascular testing (ankle‑brachial index or duplex ultrasound), neuropathy screening, review of glycemic control, nutritional assessment, and infection workup including cultures when appropriate. If a wound shows no measurable improvement in size or healthy granulation over two to four weeks, clinicians usually reassess; lack of progress by four to twelve weeks is commonly considered chronic and prompts consideration of advanced therapies and multidisciplinary care.
Why Do Chronic Wounds Stop Healing? Common Causes and Risk Factors
Wounds stop healing when local or systemic factors disrupt normal repair, keeping the wound inflamed, preventing new vessel growth, or allowing persistent microbial communities to resist treatment. Common biological contributors include a stalled inflammatory phase, high protease activity that breaks down growth factors and matrix, poor angiogenesis, and biofilm that shields bacteria from antibiotics and immune cells. Identifying which combination of barriers is present—circulatory insufficiency, hyperglycemia, infection, pressure, or nutritional deficits—lets clinicians target therapy to the mechanism and improve the chance of recovery. The table below summarizes common causes, how they block healing, and the clinical signs used to identify them.
Different causes create predictable changes in wound physiology and visible signs that guide diagnosis.
| Cause | How it disrupts healing | Clinical signs / effect on wound |
|---|---|---|
| Poor arterial perfusion | Limits oxygen and nutrient delivery, reducing angiogenesis | Pale, cool skin; slow capillary refill; pain with activity or at rest |
| Venous hypertension | Leads to edema and protein‑rich exudate that impair repair | Heavy drainage, hemosiderin staining, medial lower‑leg location |
| Diabetes / hyperglycemia | Impairs immune function and sensation, and harms microcirculation | Reduced sensation, higher infection risk, delayed granulation |
| Infection / biofilm | Maintains inflammation and resists eradication | Foul odor, increased drainage, friable tissue, stalled progress |
| Pressure / shear | Repeated mechanical trauma prevents repair | Localized redness, tissue breakdown over bony areas |
| Malnutrition / micronutrient deficits | Limits collagen production and cell proliferation | Poor granulation, slow epithelialization, muscle wasting |
This quick reference shows how causes align with treatment priorities and helps clinicians choose targeted diagnostics—vascular studies, glucose optimization, or focused debridement—to remove barriers and restart healing.
How Does Poor Circulation Affect Chronic Wound Healing?
Poor circulation—whether from arterial insufficiency or venous disease—reduces delivery of oxygen, nutrients, and immune cells that tissue repair needs. It often shows as cool skin, weak pulses, or marked leg swelling, depending on the cause. Arterial disease produces ischemic wounds that are typically painful and found on toes or pressure points; venous insufficiency causes chronic edema and inflammatory exudate that break down tissue on the lower leg. Clinicians use ankle‑brachial index testing and duplex ultrasound to quantify compromise and decide whether revascularization, compression, or edema control is appropriate. Restoring circulation creates the environment other treatments need to work.
What Role Do Diabetes and High Blood Sugar Play in Non-Healing Wounds?
Diabetes contributes to chronic wounds through peripheral neuropathy, which prevents detection of minor injuries, and through microvascular disease and immune dysfunction that blunt repair. Hyperglycemia impairs leukocyte function and collagen synthesis, raising infection risk and slowing granulation. Diabetic wounds commonly occur on plantar surfaces and pressure points. Effective care always includes optimizing blood sugar, ensuring proper offloading (pressure redistribution), and coordinating podiatric and vascular care as needed. Multidisciplinary diabetic foot programs combine metabolic control, local wound therapies, and protective footwear to improve outcomes.
How Do Infection and Biofilm Formation Prevent Healing?
Infection and biofilm keep wounds inflamed and shield bacteria from antibiotics and immune clearance, so surface cleaning alone is often insufficient. A biofilm is a community of bacteria embedded in a protective matrix that adheres to the wound bed; it blocks cell migration and breaks down growth factors needed for granulation. Clinicians separate simple colonization from invasive infection by looking for systemic signs, worsening pain, spreading redness, odor, and changes in drainage. Management commonly requires sharp debridement to remove biofilm plus targeted topical or systemic antimicrobial therapy. Breaking the biofilm and restoring a clean wound bed is frequently the turning point toward visible progress.
Biofilm Management Strategies for Non-Healing Chronic Wounds
Recognizing bacterial biofilm as a major driver of non‑healing wounds means treatment must include biofilm‑targeted steps. Standard care elements—systemic and topical antimicrobials, antiseptics, and physical debridement of biofilm and devitalized tissue—remain important, but focused strategies to disrupt biofilm improve outcomes.
What Other Factors Contribute to Chronic Wound Non-Healing?
Beyond circulation, diabetes, and infection, several modifiable and non‑modifiable factors prolong wounds by impairing repair or repeatedly injuring tissue. Protein and micronutrient deficiencies (vitamin C, zinc) limit collagen synthesis and cell growth. Ongoing pressure or shear re‑injures vulnerable areas. Some medications—especially systemic steroids—suppress needed inflammatory responses. Smoking and obesity reduce perfusion and increase inflammation, and age‑related changes in skin and immunity slow healing. A comprehensive plan addresses nutrition, pressure relief, medication review, smoking cessation, and realistic activity changes to remove ongoing barriers and support recovery.
When Should You Seek Advanced Wound Care? Signs and Symptoms to Watch For
Knowing when to escalate from basic care to specialist evaluation is critical—early targeted interventions reduce complications and improve healing chances. Seek advanced care for increased pain, spreading redness or warmth, new or worsening odor or drainage, failure to show measurable improvement after two to four weeks, or any systemic symptoms like fever or malaise. Immediate urgent evaluation is needed for exposed bone, tendon, or implants; rapidly enlarging wounds; uncontrolled bleeding; or signs of systemic infection. For patients and caregivers, tracking wound photos, measurements, and daily symptoms helps clinicians decide whether a referral to advanced wound care is timely.
When these warning signs appear, a mobile assessment can be a practical next step for patients who have trouble traveling or need prompt hands‑on evaluation. Healix360 Advanced Mobile Wound Care Specialists provides in‑home and on‑site assessments that mirror clinic care—measuring wounds, performing vascular screening when appropriate, obtaining cultures, and beginning treatments like debridement or dressing changes at home. This mobile workflow reduces delays for homebound patients and lets clinicians start targeted therapies sooner, often changing the wound’s trajectory toward healing.
What Are the Warning Signs of a Non-Healing or Complicated Wound?
Patients and caregivers should watch for clear changes that signal complication and need for clinician attention: increasing pain, swelling, spreading redness or red streaks, new or worsening foul odor, and increased or purulent drainage. Systemic signs—fever, chills, rising blood glucose, or marked fatigue—suggest invasive infection and require urgent evaluation. Loss of function, new bleeding, or visible bone or tendon exposure are immediate red flags. If any of these occur, stop routine home dressing changes and contact a wound care provider promptly to prevent progression.
How Long Is Too Long for a Wound to Heal Before Getting Specialist Care?
Use time thresholds as guidance: lack of measurable improvement in wound size or quality after two to four weeks should prompt reassessment. Persistent non‑progression by four to twelve weeks is commonly considered chronic and often requires advanced therapies. Measurable improvement includes reduced surface area, healthier granulation tissue, or less exudate; if these aren’t present within two to four weeks, the initial approach may be insufficient. Exceptions apply—rapidly worsening wounds, severe ischemia, exposed structures, or systemic infection need immediate specialist or hospital care regardless of timeline. Clear timelines plus symptom tracking enable timely escalation and help prevent avoidable complications.
What Are the Benefits of Advanced Mobile Wound Care for Chronic Wounds?
Advanced mobile wound care brings specialist assessment and treatments into the home, reducing access barriers and enabling consistent, timely interventions that support healing and lower complication risk. Mobile specialists can perform comprehensive evaluations, apply advanced dressings or biologic grafts, manage negative pressure wound therapy devices, and teach patients and caregivers—reducing travel strain and hospital exposure. Many patients find home care increases adherence and allows more frequent, comfortable follow‑up, which correlates with better outcomes. In some cases, advanced regenerative and graft treatments delivered at home may qualify for Medicare Part B coverage for eligible patients, improving affordability.
The table below shows how mobile service features translate into patient‑centered impact with practical examples.
| Service Feature | Patient Impact | Practical Example |
|---|---|---|
| In-home specialist visits | Less travel and better adherence | Homebound patient receives weekly dressing change and NPWT monitoring |
| Advanced regenerative options | Faster tissue repair with fewer clinic trips | Amniotic membrane graft applied at home to encourage granulation |
| Weekly follow-up cadence | Early detection of setbacks and timely changes | Specialist adjusts dressings based on weekly photodocumentation |
| Medicare Part B coverage (when applicable) | Potentially lower out‑of‑pocket costs for eligible therapies | Eligible patient receives documented, covered biologic graft |
Negative pressure wound therapy (NPWT) is a well‑established option with demonstrated benefit across many chronic wound types.
Negative Pressure Wound Therapy: Clinical Applications for Chronic Wounds
Vacuum‑assisted closure has shown effectiveness in managing diabetic foot ulcers, pressure injuries, chronic wounds, and skin grafts by promoting granulation and controlling exudate.
How Does In-Home Mobile Wound Care Improve Patient Comfort and Accessibility?
In‑home care removes transport and mobility barriers that often delay wound management, making it easier for older adults and patients with limited mobility to receive regular, timely treatments. The home setting can reduce anxiety, let caregivers participate directly in teaching, and allow clinicians to assess real‑world factors—pressure points, footwear, and home hygiene—that affect healing. To prepare for a mobile visit, clear a small workspace, have recent wound photos or notes ready, and make sure the patient can be positioned comfortably for assessment. Providing care where the patient lives improves continuity, reduces missed visits, and supports adherence to complex regimens.
What Expertise Do Mobile Wound Care Specialists Provide?
Mobile wound care specialists bring focused assessment skills, procedural competency, and care coordination that mirror clinic services but in the patient’s home. They evaluate vascular status, screen for neuropathy, measure wounds, perform debridement to remove nonviable tissue, apply biologic grafts like amniotic membranes, and set up or manage NPWT devices when appropriate. Specialists coordinate with referring clinicians—primary care, vascular surgery, endocrinology—to align systemic care with local wound strategies. This combination of technical skill, clear communication, and caregiver education helps integrate treatment into daily life and improves long‑term outcomes.
How Do Regenerative Treatments Accelerate Healing in Chronic Wounds?
Regenerative therapies speed healing by supplying biologic scaffolds, signaling molecules, or cells that reduce inflammation, promote new vessel growth, and provide a framework for tissue regrowth—addressing the biologic shortages that keep wounds stalled. Stem‑cell‑related approaches and amniotic membrane grafts deliver growth factors and extracellular matrix components that modulate inflammation, encourage granulation, and support re‑epithelialization. These treatments are used when standard measures fall short and are combined with infection control, debridement, and circulation optimization to maximize benefit. The table below compares key regenerative and adjunctive therapies, their mechanisms, and realistic patient expectations.
This at‑a‑glance comparison helps patients and clinicians weigh options and set realistic timelines.
| Therapy | Mechanism | Patient benefits / expected timeline / coverage notes |
|---|---|---|
| Stem-cell-related therapy | Paracrine signaling; growth factor release | Promotes angiogenesis and granulation; benefits often appear over weeks; used alongside standard care |
| Amniotic membrane grafts | Scaffold + growth factors + anti‑inflammatory components | Reduces inflammation and supports tissue scaffold; often single application with weekly follow‑up; some uses may qualify for Medicare Part B |
| Negative pressure wound therapy (NPWT) | Mechanical off‑loading; reduces edema and promotes perfusion | Prepares wound bed and encourages granulation; requires device management and regular changes |
| Biologic dressings / skin substitutes | Replace missing matrix; support cell migration | Useful for large or complex defects; choice depends on wound characteristics |
What Is Stem Cell Therapy and How Does It Promote Wound Healing?
Stem‑cell‑related approaches aid repair mainly through paracrine signaling: cells or cell‑derived products release growth factors and cytokines that modulate inflammation, recruit native repair cells, and stimulate angiogenesis. The result is faster granulation, reduced chronic inflammation, and improved tissue quality that supports closure. In practice, these therapies are applied alongside debridement and infection control, with regular follow‑up to monitor integration and healing. Healix360’s mobile delivery model allows assessment, application, and follow‑up to occur in the patient’s home, which can make the process more comfortable and easier for caregivers to manage.
How Do Amniotic Membrane Grafts Work and What Are Their Patient Benefits?
Amniotic membrane grafts act as a biologic scaffold rich in growth factors and anti‑inflammatory molecules that protect the wound bed and actively promote tissue regeneration with minimal bulk and straightforward application. Clinically, these grafts reduce local inflammation, provide a matrix for cell migration, and support granulation and epithelialization—often in an outpatient or in‑home setting.
For patients, benefits can include fewer dressing changes, reduced wound pain, and potential Medicare Part B coverage for qualifying applications with appropriate documentation. Evidence shows improved healing rates for selected chronic wounds when these grafts are used as part of a comprehensive plan.
What Other Advanced Therapies Support Chronic Wound Healing?
A variety of adjunctive therapies complement regenerative options and target different barriers to healing. Debridement methods—sharp, enzymatic, and autolytic—remove nonviable tissue and biofilm to create a healthy wound bed. NPWT controls exudate, reduces edema, and stimulates granulation. Bioengineered skin substitutes and topical antimicrobials replace missing matrix or manage local bioburden. Adjunctive options such as hyperbaric oxygen therapy may be considered for refractory ischemic or radiation‑injured tissue. Telehealth and remote monitoring also help maintain close surveillance and enable timely plan adjustments.
How Can Patients and Caregivers Support Healing and Manage Chronic Wounds at Home?

Patients and caregivers are central to daily wound management: following dressing instructions, offloading pressure, watching for infection, managing pain, and maintaining nutrition all directly affect healing. Clear routines for dressing changes, hand hygiene, and protected activity reduce reinjury and infection risk. Symptom logs and wound photos help clinicians make decisions between visits. Pain control and correct medication use enable mobility and participation in care, while adequate protein and key micronutrients support the body’s repair needs. Regular follow‑up and open communication with clinicians ensure small changes are caught early and treatment plans are adjusted promptly.
What Are the Key Steps for Managing Pain, Infection Risk, and Wound Care at Home?
A practical home‑care checklist helps caregivers implement daily measures that support healing and recognize when to escalate care. Key steps include keeping dressings clean and dry per clinician instructions, photographing and documenting wound size and appearance, minimizing pressure through offloading or repositioning, taking prescribed antibiotics and pain medications correctly, and attending nutritional counseling if recommended. Watch for increased drainage, odor, spreading redness, fever, or new pain and contact the wound team promptly if these signs appear. Safety cautions: avoid unapproved topical remedies, don’t attempt aggressive self‑debridement, and follow device instructions for therapies such as NPWT.
How Does Healix360 Support Caregivers Through Communication and Treatment Plans?
Healix360 Advanced Mobile Wound Care Specialists use a predictable communication rhythm and caregiver‑friendly documentation to reduce stress and improve adherence. Typical in‑home service begins with an initial assessment followed by weekly follow‑ups that review wound progress, dressing changes, pain control, and device management as needed. Specialists provide photodocumentation, written notes for the primary clinician, and clear instructions for caregivers. Coordination with referring physicians ensures systemic issues—glucose control, vascular referrals, or nutritional needs—are addressed alongside local care. Remote check‑ins or messaging let caregivers report concerns between visits. This structured approach supports caregivers with education, timely adjustments, and reassurance throughout the healing process.
- Daily hygiene and dressing protocol: Follow clinician‑specified steps for cleaning and dressing the wound to lower infection risk.
- Offloading and pressure relief: Use recommended devices or positioning strategies to remove pressure from the wound area.
- Symptom tracking and photodocumentation: Record size, drainage, odor, and pain daily and share photos during follow‑ups.
These practical tasks, paired with regular clinician contact, keep care aligned with treatment goals and allow rapid responses to setbacks—improving the likelihood of sustained healing.
Frequently Asked Questions
What lifestyle changes can help improve chronic wound healing?
Simple, targeted lifestyle changes can meaningfully improve healing. Stop smoking—tobacco impairs circulation and delays repair. Eat a balanced diet with adequate protein, vitamin C, zinc, and other key nutrients to support tissue rebuilding. Stay as active as health allows to improve circulation. Manage stress through breathing, relaxation, or counseling, since chronic stress can affect immune function. Work with your healthcare team to build a personalized plan that addresses these factors.
How can caregivers effectively monitor chronic wounds at home?
Caregivers can help by creating a daily routine for wound checks: note changes in size, color, drainage, and odor, and look for signs of infection such as increased pain or swelling. Keep a simple log with dates and photos to track progress. Share concerns with the wound team promptly—early reporting leads to faster problem solving and better outcomes.
What are the potential complications of untreated chronic wounds?
Untreated chronic wounds can lead to serious complications, including spreading infections and sepsis, osteomyelitis (bone infection), extensive tissue loss that may require surgery or amputation, prolonged pain, and reduced quality of life. Early, appropriate care reduces these risks and improves the chance of recovery.
What role does patient education play in chronic wound management?
Patient education is essential. Understanding the wound, following the treatment plan, and recognizing warning signs empower patients to take an active role in healing. Education covers proper wound care techniques, nutrition, activity modification, and when to seek help. Engaged patients typically follow plans more closely and have better outcomes.
How do advanced therapies differ from traditional wound care methods?
Advanced therapies—like NPWT and regenerative treatments—go beyond basic dressings and topical ointments by addressing underlying biological barriers to healing. NPWT helps remove excess fluid and stimulates granulation. Regenerative therapies supply growth factors and matrix elements that promote tissue repair. These options are often used when standard approaches fail and are part of a more comprehensive strategy for complex wounds.
What should patients expect during a mobile wound care visit?
During a mobile visit, a specialized clinician performs a focused assessment in the patient’s home: measures the wound, inspects surrounding tissue, and checks for infection or complications. Treatments may include debridement, advanced dressings, or device setup. Patients receive education on care, pain management, and next steps, and follow‑up visits are scheduled to monitor progress and adjust treatment.
How can technology assist in chronic wound management?
Technology enhances monitoring and communication. Telehealth lets patients consult specialists remotely, cutting travel and enabling timely advice. Mobile apps can track wound photos, symptoms, and medications, improving handoffs to clinicians. Some advanced devices include smart features that report status to providers, helping teams respond faster and keep care on track.
Conclusion
Understanding what stops wounds from healing and knowing when to seek advanced care helps patients and caregivers make informed choices that improve outcomes. Mobile wound care brings specialist skills and advanced treatments into the home when needed, speeding access and reducing barriers to care. Paired with lifestyle changes and clear communication with clinicians, a comprehensive approach gives the best chance of recovery. Explore our resources to learn more about optimizing chronic wound care and take the next step toward healing today.







