Wound assessment — a practical guide to advanced mobile and chronic wound evaluation
Assessing a wound correctly is the first step toward better healing. This guide walks through the practical steps clinicians and caregivers use to evaluate wounds, spot early signs of infection, and decide on next steps. It also explains how mobile wound care—delivered in the home or facility—can remove barriers to specialized treatment. Many people live with chronic wounds that need focused, ongoing attention; accurate assessment helps build tailored plans that speed recovery and reduce complications. Below we cover assessment steps, complication recognition, and how advanced mobile teams like Healix360 deliver care where patients are most comfortable.
There is growing evidence that mobile health and remote assessment can improve outcomes for people with chronic wounds.
Mobile health for remote chronic wound assessment
Remote assessment and management of wounds via mobile and telehealth methods can ease the burden on patients and caregivers and lead to better outcomes. Capturing clear wound images is central to documentation, since poor image quality reduces assessment reliability.
Wound image quality from a mobile health tool for home-based chronic wound management with real-time quality feedback: randomized feasibility study, J Zhang, 2021
Essential steps in a thorough wound assessment
A reliable wound assessment follows a clear sequence: gather the patient’s history, inspect the wound, measure its dimensions, classify the wound-bed tissue, and record findings precisely. This structured process guides clinical decisions and keeps the care team aligned over time.
Measuring and documenting wound size and depth
Accurate measurements are key to judging progress. Clinicians usually measure length, width and deepest point with a ruler or tape measure, then record those numbers in the chart. Consistent technique and careful notes let teams spot meaningful changes and act quickly when healing stalls.
Recognizing wound-bed tissue types
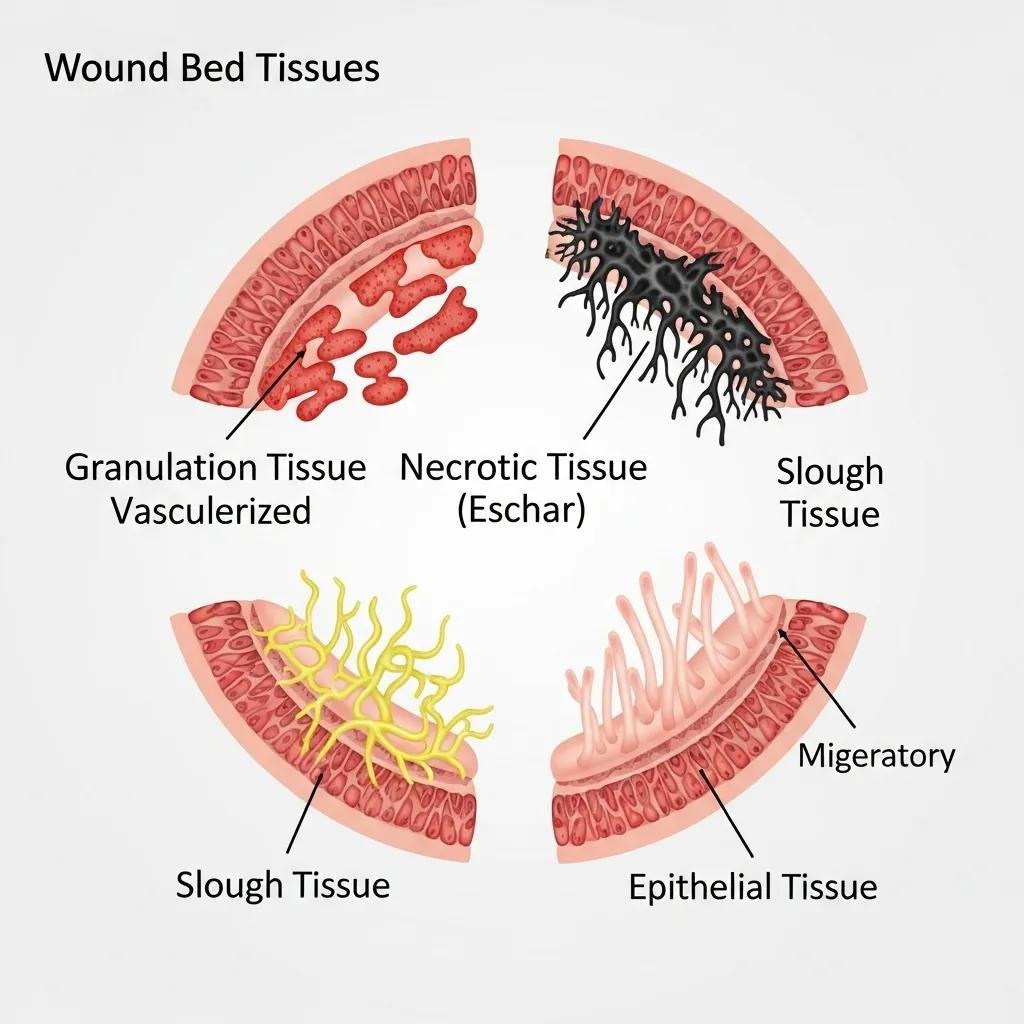
Identifying the tissue in the wound bed directs treatment. Granulation tissue is pink or red and moist — a sign of healthy repair. Necrotic tissue may appear black, brown or yellow and needs removal. Slough is often yellow or white and can be stringy or moist. Epithelial tissue is pale and indicates the wound is resurfacing. Clear description of each tissue type helps clinicians choose debridement, dressings, or other targeted therapies.
Spotting infection and other complications during evaluation
Early detection of infection or complication changes the plan of care. During every assessment, clinicians look for signs that suggest microbial invasion or tissue breakdown so treatment can be started without delay.
Common signs of wound infection
Watch for these common indicators:
- Redness: Inflamed skin around the wound.
- Warmth: The wound area feels warmer than surrounding skin.
- Swelling: Increased tissue swelling or puffiness.
- Pain or tenderness: New or worsening discomfort.
- Discharge: Purulent fluid or unusual exudate.
- Foul odor: Persistent bad smell suggesting bacterial activity.
- Delayed healing: Lack of expected progress over time.
Noticing these signs early enables prompt interventions that limit spread and support recovery.
Periwound skin assessment to detect complications
Examining the skin around the wound — the periwound — reveals problems before they worsen. Look for maceration, redness tracking away from the wound, breakdown from pressure, or other changes. Simple inspection and gentle palpation inform dressing choices and help prevent secondary skin damage.
Why Healix360’s mobile wound assessments are effective

Mobile wound care brings specialist expertise to the patient’s home or care setting. Healix360 combines experienced clinicians, standardized assessment protocols, and modern imaging to provide focused evaluations and clear treatment plans without the stress of repeated clinic visits. That convenience improves access and keeps care consistent.
How Healix360 provides expert in-home and facility-based assessments
Our team of trained wound specialists visits patients in their homes and care facilities to perform full assessments, document findings, and create individualized care plans. We coordinate with primary clinicians and caregivers so the plan fits each patient’s needs and environment — helping wounds move toward recovery with targeted interventions.
Adding mobile technologies like 3D imaging can increase the precision and repeatability of home-based assessments.
3D mobile imaging for accurate wound assessment
Structured-light sensors and related methods enable reliable three-dimensional wound measurement. Proper system design supports fast, repeatable cutaneous wound assessment on low-cost mobile devices.
System design for 3
D wound imaging using low-cost mobile devices, E Sirazitdinova, 2017
Technologies and tools used in mobile wound evaluation
Mobile wound teams use digital photography and imaging tools for precise measurements, telehealth platforms for specialist input, and advanced dressings that support healing. Integrating these tools helps clinicians track progress objectively and select treatments that match the wound’s current needs.
Advances in mobile imaging offer clear advantages over traditional remote methods for wound assessment.
Mobile imaging for remote wound assessment
Many commercially available wound-assessment systems now rely on mobile imaging. These systems often outperform older, traditional imaging devices for remote monitoring and documentation.
Wound assessment, imaging and monitoring systems in diabetic foot ulcers:
A systematic review, KS Chan, 2020
How assessment guides advanced regenerative treatment planning
A careful assessment frames choices about regenerative therapies. By reviewing wound type, size, depth, tissue quality and infection status alongside the patient’s overall health, clinicians can recommend targeted biologic or cellular therapies when appropriate.
Choosing stem cell therapy and biologic dressings from the assessment
Selection of stem cell treatments or biologic dressings follows a clinical evaluation. Factors such as wound chronicity, tissue type, infection control and patient comorbidities determine whether regenerative options will add benefit. When chosen thoughtfully, these therapies create a healing environment and encourage tissue repair.
The role of debridement and negative pressure therapy
Debridement removes devitalized tissue that blocks healing and reduces infection risk. Negative pressure wound therapy (NPWT) applies controlled suction to promote blood flow and granulation tissue formation. Both are evidence-based tools whose use is guided by findings from the initial assessment and ongoing progress checks.
What are the stages of wound healing and how are they assessed?
Understanding the healing stages helps clinicians interpret findings and adjust care. Wounds typically progress through hemostasis, inflammation, proliferation and remodeling — each with distinct signs and timelines that inform treatment choices.
The inflammatory, proliferative and remodeling phases explained
The inflammatory phase is the immediate response to injury and includes redness, swelling, warmth and pain; it usually lasts days. The proliferative phase follows, with new tissue formation and wound contraction. Remodeling is the long-term phase when tissue strengthens and matures; this can continue for months to years. Recognizing each phase ensures interventions support — rather than disrupt — recovery.
How monitoring healing progress shapes treatment
Regular, consistent assessments let clinicians see whether therapies are working or need a change. Tracking wound dimensions, tissue type and symptoms over time guides timely adjustments and helps avoid unnecessary treatments.
How caregivers can support wound assessment and healing at home
Caregivers are vital partners in wound care. Their daily observations and routine care make a big difference in outcomes and in keeping clinicians informed between visits.
Practical tips for caregivers to monitor and report wound changes
Helpful practices for caregivers include:
- Regular inspections: Check the wound daily for changes in color, drainage, or skin condition.
- Document changes: Keep a simple log of size, smell, color, and any new symptoms to share with the care team.
- Maintain cleanliness: Follow dressing and hygiene instructions to reduce infection risk.
These habits improve communication with clinicians and support timely interventions.
Why patient education improves wound care outcomes
When patients and caregivers understand wound goals, dressing routines, and warning signs, they follow care plans more reliably. Clear educational materials — checklists, short videos, and step-by-step guides — boost adherence and help prevent avoidable setbacks.
| Wound Type | Typical features | Treatment Options |
|---|---|---|
| Diabetic Foot Ulcers | Often deep, with risk of infection | Advanced dressings, debridement, offloading, glycemic control |
| Pressure Ulcers | Localized skin and tissue damage from pressure | Regular repositioning, moisture management, specialized dressings |
| Venous Leg Ulcers | Shallow, often irregular margins with persistent exudate | Compression therapy, wound dressings, treating venous insufficiency |
In summary, thorough wound assessment combines careful observation, consistent measurement, and the right use of technology and therapies. Mobile wound-care teams like Healix360 help bring that expertise to patients’ homes, improving convenience and continuity of care. With precise assessments, timely interventions and engaged caregivers, the path to recovery becomes clearer and faster.
Frequently asked questions
What are the benefits of using mobile wound care services?
Mobile wound care reduces travel and disruption for patients while delivering specialized assessment and treatment where they live. It increases access to expert clinicians, promotes consistent follow-up, and often leads to better comfort, adherence and outcomes.
How can technology improve wound assessment accuracy?
Digital tools — from high-quality photos to 3D imaging and telehealth platforms — make measurements more objective and repeatable. They support remote specialist input and better documentation, helping clinicians choose the right treatment sooner.
What role do caregivers play in wound healing?
Caregivers monitor daily changes, maintain dressing routines, and communicate observations to clinicians. Their attention to hygiene, documentation and symptom reporting is critical to preventing complications and keeping treatment on track.
What are the common challenges in wound assessment?
Challenges include varied wound presentations, patient comorbidities that slow healing, and inconsistent image quality during remote assessments. Clear training, standardized protocols, and robust imaging tools help overcome these hurdles.
How does patient education impact wound care?
Education empowers patients and caregivers to follow care plans correctly, recognize warning signs early, and engage with clinicians proactively. Better-informed patients typically see faster recovery and fewer complications.
What are the signs that a wound is healing properly?
Signs of good healing include gradual reduction in wound size, healthy granulation tissue, less pain and swelling, and absence of foul odor or excessive discharge. Regular monitoring helps confirm steady progress.
Conclusion
Accurate wound assessment is the foundation of effective, personalized care. By combining clinical expertise, consistent measurement, caregiver engagement and mobile technologies, teams like Healix360 help patients heal with dignity and fewer disruptions. Learn more about how our solutions can support your healing journey today.







